Bioethics Exam Questions and Answers Guide
Understanding Bioethics in Modern Medicine
Key Ethical Issues in Healthcare
Common Bioethics Exam Topics
Principles of Medical Ethics Explained
How to Approach Ethical Dilemmas
Important Theories in Bioethics
Case Studies for Bioethics Exams
Ethical Considerations in Genetic Testing
The Role of Informed Consent in Healthcare
Challenges in Organ Donation Ethics
Bioethics in End-of-Life Decisions
Environmental Bioethics and Public Health
The Impact of Technology on Ethics
Ethical Issues in Reproductive Rights
Animal Research and Ethical Concerns
Preparing for Bioethics Exam Questions
Answering Bioethics Exam Questions Effectively
Bioethics Exam Questions and Answers
Preparing for tests in ethics related to medical practices requires understanding complex moral issues that influence modern healthcare decisions. These topics explore critical dilemmas in medicine, genetics, and technology, pushing students to think deeply about the consequences of choices in life-and-death situations.
Key Areas to Focus On
- Fundamental principles of medical ethics
- Ethical challenges in patient consent
- Debates surrounding end-of-life care
- The ethics of genetic research and testing
- Animal rights in medical research
Effective Study Tips
- Review case studies that showcase real-world dilemmas
- Practice articulating your views clearly and logically
- Understand the legal and moral boundaries in healthcare
- Discuss ethical theories to apply them to scenarios
- Keep updated on current debates and advances in medicine
Understanding Bioethics in Modern Medicine
In contemporary healthcare, professionals face a variety of moral challenges that require careful thought and judgment. These ethical issues often arise from the use of new technologies, medical interventions, and the evolving understanding of human rights. The decisions made in these areas can profoundly impact individuals, communities, and society as a whole.
Ethical dilemmas in medicine frequently involve balancing patient well-being with professional responsibility. The application of cutting-edge technologies, such as genetic testing and artificial intelligence, brings new questions about privacy, consent, and fairness. As medical practice continues to evolve, the need for ethical frameworks that guide these decisions becomes increasingly important.
Modern healthcare also introduces concerns about access to treatments, especially in situations where resources are limited. For example, how should scarce medical resources be allocated? Who decides what treatments are necessary or ethical in life-threatening circumstances? These questions reflect broader societal concerns that influence medical practice.
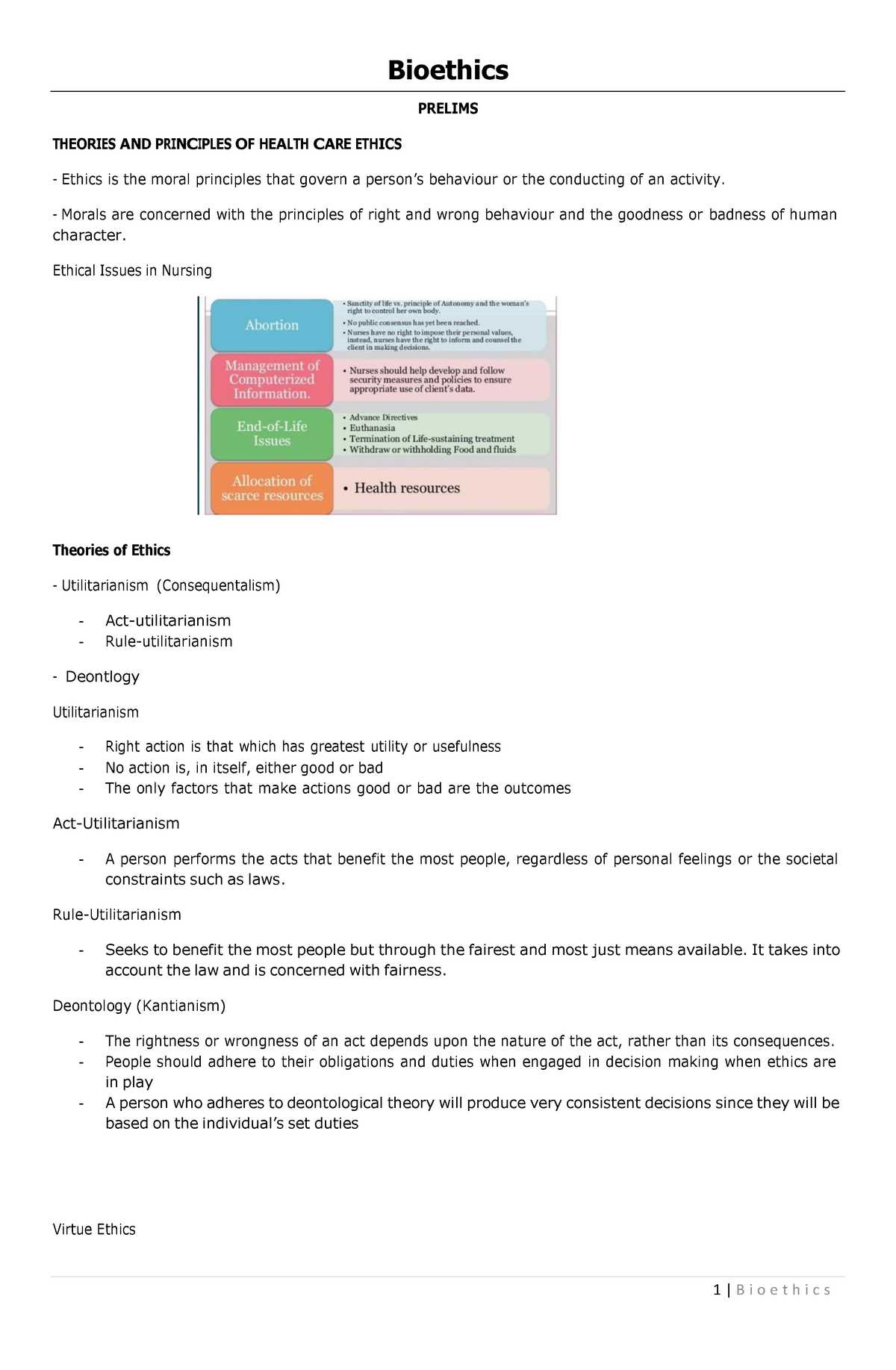
Key Ethical Issues in Healthcare
Healthcare is filled with complex moral challenges that demand thoughtful analysis. Professionals must navigate situations where the interests of patients, families, and society can sometimes conflict. These ethical dilemmas are crucial to understanding the broader responsibilities of those in the medical field and ensuring decisions are made with integrity and fairness.
- Patient autonomy: Respecting individuals’ rights to make decisions about their own health care, even when those choices may differ from what medical professionals recommend.
- Informed consent: Ensuring that patients fully understand the risks, benefits, and alternatives of treatments before agreeing to any procedure.
- Confidentiality: Protecting patient privacy and maintaining trust by safeguarding sensitive medical information.
- Resource allocation: Deciding how to fairly distribute limited resources, especially in critical situations where there may be more patients than available treatment.
- End-of-life care: Navigating decisions around life-support, euthanasia, and palliative care, often involving deeply personal and cultural considerations.
Common Bioethics Exam Topics
When preparing for assessments on healthcare ethics, it’s essential to focus on the most prevalent topics that often appear in discussions. These subjects typically involve pressing moral issues in modern medicine, which require a deep understanding of both theoretical concepts and practical applications. Below are several key areas commonly addressed in this field.
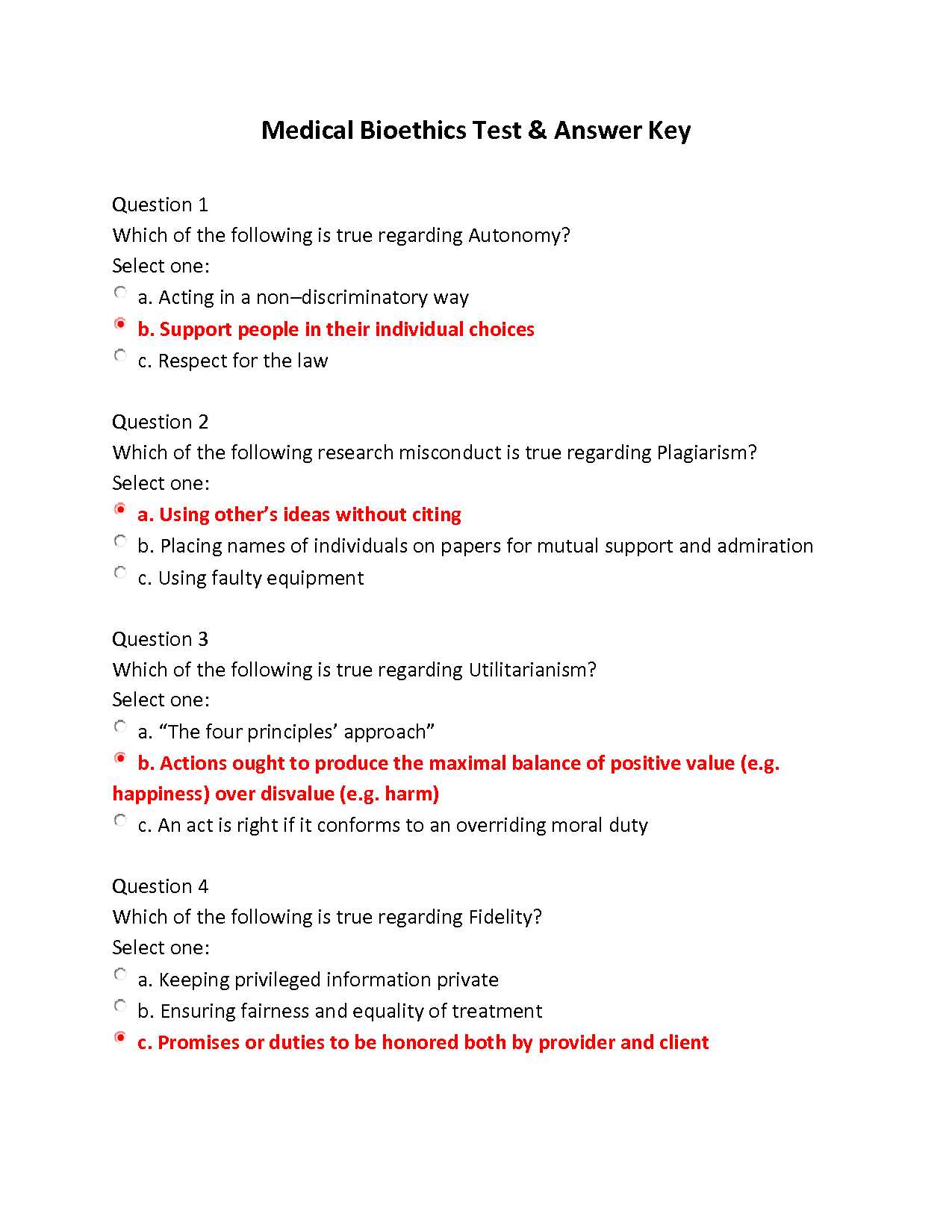
Fundamental Ethical Principles
- Autonomy: The right of individuals to make decisions about their own health care.
- Beneficence: The obligation to act in the best interest of patients.
- Non-maleficence: The duty to do no harm to patients.
- Justice: The fair distribution of healthcare resources.
Real-World Dilemmas in Healthcare
- Genetic testing: Ethical concerns related to privacy, consent, and the potential for discrimination.
- End-of-life decisions: Issues such as euthanasia, assisted suicide, and the right to refuse treatment.
- Organ transplantation: Ethical challenges in organ donation, allocation, and transplantation.
- Reproductive rights: Moral considerations surrounding abortion, fertility treatments, and family planning.
Principles of Medical Ethics Explained
The foundation of healthcare decision-making lies in a set of ethical principles that guide professionals in making choices that protect patient rights, promote well-being, and ensure fairness. These core values are essential for maintaining trust between healthcare providers and patients while navigating complex moral situations. Understanding these principles is crucial for making informed and responsible decisions in medical practice.
Core Ethical Values in Healthcare
- Autonomy: Respecting a patient’s right to make informed decisions about their own health and treatment options.
- Beneficence: Acting in the best interest of the patient by promoting their health and well-being.
- Non-maleficence: The principle of “do no harm,” ensuring that medical actions do not cause unnecessary injury or suffering.
- Justice: Ensuring fairness in the distribution of healthcare resources and equal treatment for all patients.
Applying Ethics to Complex Scenarios
- Informed consent: Ensuring that patients understand the risks and benefits of medical procedures before agreeing to them.
- Confidentiality: Safeguarding patient privacy and protecting sensitive health information from unauthorized disclosure.
- Resource allocation: Making ethical decisions on how to distribute limited healthcare resources, particularly in emergencies.
How to Approach Ethical Dilemmas
When faced with challenging moral decisions in healthcare, it’s essential to carefully evaluate all aspects of the situation. Professionals must consider the values, potential consequences, and the interests of all parties involved. An ethical decision-making process helps ensure that choices are made with integrity and respect for both the individual and societal well-being.
Step 1: Identify the core issue – The first step in tackling any dilemma is to clearly define the ethical conflict. Understand the nature of the problem and what makes it ethically complex.
Step 2: Gather relevant information – Collect all pertinent facts and context about the situation. This may include medical history, patient preferences, legal constraints, and any available research or guidelines.
Step 3: Evaluate the options – Consider the possible courses of action. Reflect on how each choice aligns with ethical principles, such as respect for autonomy, beneficence, non-maleficence, and justice.
Step 4: Make an informed decision – After careful consideration, select the option that best balances ethical principles while minimizing harm and respecting patient rights.
Step 5: Reflect and learn – After resolving the dilemma, take time to reflect on the decision-making process. Consider what was learned and how it might apply to future ethical challenges.
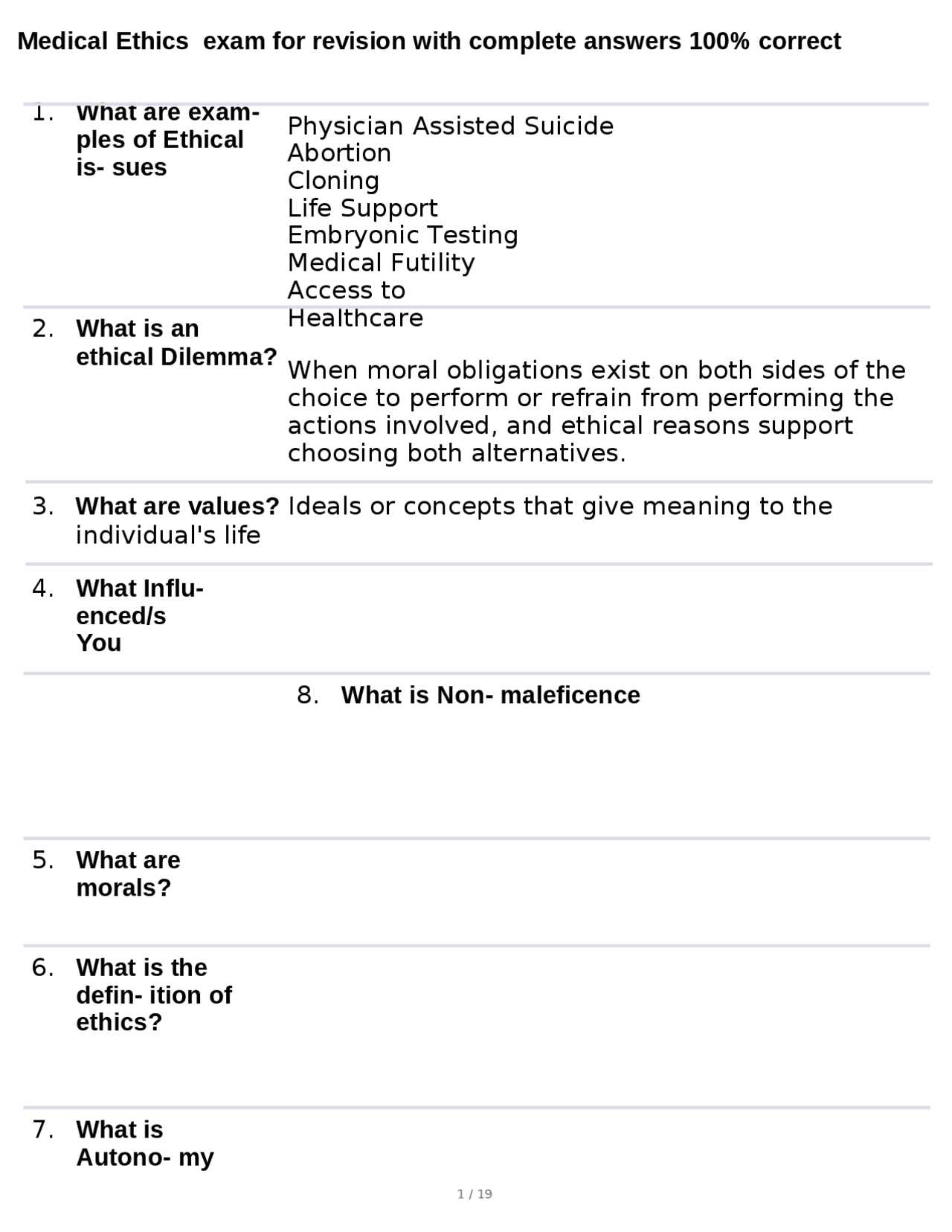
Important Theories in Bioethics
In the realm of healthcare decision-making, several moral theories provide frameworks for resolving complex ethical issues. These theories help guide professionals in determining the right course of action when faced with challenging dilemmas. Understanding the key ethical models is essential for making well-reasoned and just decisions in medical practice.
- Utilitarianism: This theory suggests that the most ethical action is the one that produces the greatest good for the greatest number. It emphasizes outcomes and focuses on maximizing overall well-being.
- Deontological Ethics: Rooted in the work of Immanuel Kant, this approach asserts that actions are morally right if they follow a set of rules or duties, regardless of the consequences.
- Virtue Ethics: This theory emphasizes the importance of moral character and virtues, rather than focusing solely on the actions themselves. It suggests that individuals should strive to become good people and make decisions based on the qualities of a virtuous character.
- Care Ethics: This approach highlights the importance of relationships and care in ethical decision-making. It emphasizes empathy, compassion, and the context of human relationships in determining what is morally right.
- Principlism: Common in healthcare ethics, this model focuses on four key principles: autonomy, beneficence, non-maleficence, and justice. These principles guide decision-making in a variety of medical contexts.
Case Studies for Bioethics Exams
Case studies are an essential tool for exploring ethical dilemmas in healthcare. They provide practical examples of situations where moral principles come into conflict, allowing students and professionals to apply theoretical knowledge to real-world scenarios. These studies help in understanding how to navigate complex situations while balancing the interests of patients, medical staff, and society.
Example 1: Informed Consent in Surgery
A patient is scheduled for a major surgery, but they are not fully aware of the potential risks involved. The healthcare team is faced with the decision of whether to proceed with the surgery without the patient’s full understanding. This scenario raises concerns about autonomy and the right of the patient to make informed decisions about their own care.
Example 2: Resource Allocation During a Pandemic
During a health crisis, there are limited resources such as ventilators, and healthcare professionals must decide how to prioritize patients for treatment. The decision-making process involves complex ethical questions about justice and how to fairly allocate scarce resources to save as many lives as possible.
Each of these case studies highlights important ethical considerations, such as patient rights, justice, and fairness, all of which are central to understanding moral issues in healthcare. By analyzing these cases, individuals can improve their ability to make ethically sound decisions in their professional practice.
Ethical Considerations in Genetic Testing
Genetic testing raises numerous ethical concerns due to its profound impact on individuals, families, and society. It provides valuable information about inherited diseases, but it also presents complex issues regarding privacy, consent, and the potential for discrimination. Understanding these ethical challenges is crucial for both healthcare providers and patients as they navigate the decision-making process related to genetic screening and testing.
| Ethical Issue | Description |
|---|---|
| Informed Consent | Ensuring that patients fully understand the risks, benefits, and limitations of genetic tests before agreeing to undergo testing. |
| Privacy and Confidentiality | Protecting sensitive genetic information from unauthorized access or disclosure to prevent genetic discrimination by employers or insurance companies. |
| Genetic Discrimination | Concerns about the potential for individuals to be treated unfairly based on their genetic makeup, especially in employment and insurance sectors. |
| Psychological Impact | The emotional burden of learning about genetic predispositions to certain conditions, which may affect mental health and family dynamics. |
| Impact on Family Members | Genetic testing may reveal information not only about the individual but also about their relatives, raising ethical concerns about sharing or withholding this information. |
The Role of Informed Consent in Healthcare
Informed consent is a fundamental principle in healthcare, ensuring that patients have the autonomy to make educated decisions about their treatment. It involves providing individuals with all necessary information about their condition and potential treatment options, allowing them to make voluntary choices that align with their values and preferences. This process fosters trust and communication between patients and healthcare providers, promoting ethical and transparent medical practice.
Key Components of Informed Consent
- Disclosure of Information: Healthcare providers must explain the nature of the condition, the proposed treatment, potential risks, and benefits, as well as alternative options.
- Comprehension: It is vital that patients fully understand the information provided, ensuring that medical terminology is explained in an accessible manner.
- Voluntary Agreement: The decision to proceed with treatment must be made without coercion, allowing the patient to make an independent choice.
- Capacity to Decide: The patient must have the mental and emotional capacity to understand the information and make an informed decision about their care.
Challenges in the Informed Consent Process
- Language Barriers: Miscommunication may occur if patients do not speak the same language as their healthcare provider, potentially compromising their understanding.
- Cognitive Impairments: Patients with limited mental capacity or those under significant stress may struggle to process all the information necessary for informed consent.
- Time Constraints: In emergency situations, there may be insufficient time to thoroughly explain all aspects of treatment, raising ethical concerns about the adequacy of consent.
Challenges in Organ Donation Ethics
Organ donation is a critical medical practice that saves countless lives, yet it raises numerous ethical concerns. The decision to donate organs, whether made voluntarily or posthumously, involves complex moral considerations surrounding consent, allocation, and potential exploitation. Addressing these challenges is essential for ensuring that organ donation remains fair, transparent, and respectful of individuals’ rights.
One significant issue in organ donation is the concept of consent. In many cases, individuals are not fully informed about the implications of donation, or they may not have explicitly stated their wishes. Furthermore, the fairness of how organs are allocated is often questioned, as factors like social status, wealth, and medical urgency can influence who receives life-saving transplants. Ethical dilemmas also arise when considering the use of organs from vulnerable populations, raising concerns about the potential for exploitation.
These challenges highlight the need for clear ethical guidelines and transparency in organ donation policies. It is essential to balance respect for individual autonomy with the urgent demand for organs, ensuring that the system is both just and humane.
Bioethics in End-of-Life Decisions
End-of-life decisions are some of the most challenging and emotionally charged issues in healthcare. They involve complex ethical dilemmas regarding the autonomy of patients, the role of healthcare providers, and the moral implications of prolonging life versus allowing death to occur naturally. These decisions often require careful consideration of the patient’s wishes, quality of life, and the potential for suffering.
A key challenge is determining when it is appropriate to intervene medically and when it is more ethical to focus on comfort and palliative care. Another critical issue is the right of patients or their families to make decisions about life-sustaining treatments, particularly in cases of terminal illness. In some situations, the question of euthanasia or physician-assisted suicide also arises, further complicating the moral landscape of end-of-life care.
These dilemmas require a sensitive and respectful approach, with careful attention to the values and beliefs of those involved. While medical technology offers the ability to extend life, the ethical responsibility is to ensure that these decisions honor the dignity and wishes of the patient.
Environmental Bioethics and Public Health
The relationship between the environment and public health is a growing area of concern, as human actions continue to impact the natural world and, in turn, affect human well-being. Environmental challenges, such as pollution, climate change, and the depletion of natural resources, have direct consequences for the health of populations, particularly vulnerable groups. This intersection of ecological sustainability and human health raises important ethical questions about responsibility, equity, and justice in addressing these global issues.
The Impact of Environmental Changes on Health
Environmental degradation contributes to numerous health issues, including respiratory diseases, waterborne illnesses, and mental health challenges. Communities living in polluted areas or those affected by natural disasters often experience higher rates of chronic illness and premature death. The ethical consideration here is how to balance economic development with the health and well-being of populations, ensuring that those who are most vulnerable receive the support and resources they need to thrive.
Ethical Responsibility in Environmental Stewardship
Governments, industries, and individuals all play a role in protecting the environment. However, there are often competing interests, such as economic growth versus environmental conservation, that complicate decision-making. Ethical principles demand that actions taken today do not harm future generations and that public health is prioritized alongside economic considerations. This requires a commitment to sustainable practices and the fair distribution of resources, particularly for marginalized and at-risk communities.
The Impact of Technology on Ethics
Advancements in technology have fundamentally transformed many aspects of life, from healthcare to communication. While these innovations offer significant benefits, they also introduce new ethical challenges. As technology continues to evolve, it raises questions about privacy, autonomy, fairness, and the potential for misuse. Understanding the ethical implications of these changes is essential to navigating the complexities they bring to society.
Key Ethical Challenges in Technology
- Privacy Concerns: The rise of digital data collection and surveillance technologies has led to concerns about personal privacy. How much should individuals sacrifice for convenience and safety?
- Artificial Intelligence: As AI becomes more integrated into decision-making processes, questions arise about accountability, bias, and the potential loss of human control in critical areas like healthcare and law enforcement.
- Automation and Employment: The automation of jobs through robotics and AI creates ethical dilemmas regarding unemployment, wealth distribution, and the future of work.
Addressing Ethical Concerns in Technology
To ensure that technological progress is aligned with ethical standards, it is crucial to implement regulations and policies that protect individuals and communities. This includes creating transparent systems for data usage, ensuring fairness in AI algorithms, and fostering responsible innovation that prioritizes human well-being over profit. Continuous dialogue between technologists, policymakers, and ethicists is necessary to balance the benefits of technology with its potential risks.
Ethical Issues in Reproductive Rights
Reproductive rights encompass a range of complex ethical issues that touch on personal autonomy, social justice, and healthcare. These concerns often involve the delicate balance between an individual’s right to make decisions about their body and the interests of society at large. As reproductive technologies and policies evolve, so too do the ethical dilemmas surrounding topics such as access to healthcare, gender equality, and the moral implications of life choices.
Key Ethical Dilemmas
- Autonomy vs. Regulation: One of the central ethical debates is whether individuals should have the autonomy to make decisions about their reproductive health or if such decisions should be subject to government regulations, especially in the case of abortion or assisted reproduction.
- Access to Reproductive Healthcare: Inequities in access to reproductive services, including contraception, prenatal care, and abortion, raise ethical concerns about fairness and the right to equitable healthcare for all individuals, regardless of socio-economic status.
- Reproductive Technologies: Advances in fertility treatments, surrogacy, and genetic testing have raised questions about the ethical boundaries of intervention in human reproduction. Issues such as consent, potential exploitation, and the long-term consequences of genetic modifications are central to this debate.
Balancing Rights and Responsibilities
Ethical considerations in reproductive rights require a careful balance between individual freedoms and societal responsibilities. It is essential to address the needs and rights of women, families, and marginalized groups while also considering the potential implications of reproductive technologies and policies on future generations. Thoughtful, inclusive policies that respect individual rights and promote fairness in access to healthcare are vital in addressing these ongoing ethical challenges.
Animal Research and Ethical Concerns
The use of animals in scientific research has been a topic of intense debate, particularly when it comes to the ethical implications of such practices. While animal testing has contributed to significant advancements in medicine, pharmacology, and other scientific fields, it raises important questions about the morality of using animals for experimentation. Ethical concerns center around issues of animal welfare, consent, and the potential for unnecessary harm or suffering.
Key Ethical Issues in Animal Research
| Issue | Description |
|---|---|
| Animal Welfare | The protection of animals from unnecessary pain, distress, or suffering during research procedures is a primary ethical concern. Striking a balance between scientific progress and animal well-being is crucial. |
| Necessity of Use | One major question is whether animal testing is truly necessary or if alternatives, such as in vitro or computational models, could be used instead to achieve the same research goals. |
| Speciesism | Another ethical dilemma involves the concept of speciesism, which suggests that the interests of animals are often overlooked or undervalued compared to human interests, raising concerns about fairness and equality. |
| Long-term Impact | The long-term consequences of animal research on ecosystems, animal populations, and biodiversity also need to be considered in the ethical discussion surrounding experimentation. |
Ethical Guidelines and Regulation
To address these concerns, many countries have implemented strict regulations regarding animal research, requiring researchers to adhere to ethical guidelines that ensure the humane treatment of animals. The “3Rs” principle–Replacement, Reduction, and Refinement–aims to minimize animal use, reduce the number of animals required, and refine techniques to make experiments less invasive. However, despite these efforts, the debate continues about the moral justifiability of animal research in the context of advancing scientific knowledge.
Preparing for Ethical Assessments
Preparing for assessments in the field of ethical decision-making requires a clear understanding of key concepts, theories, and real-world applications. It is crucial to develop a methodical approach to studying, focusing not only on memorizing facts but also on analyzing complex scenarios. Mastery of the foundational principles and the ability to apply them to diverse situations are essential for success in these evaluations.
Key Areas to Focus On
- Ethical Theories – Understanding different approaches such as utilitarianism, deontology, and virtue ethics will provide a strong theoretical foundation.
- Case Studies – Analyzing real-life case studies will help in applying theoretical knowledge to practical situations and improve problem-solving skills.
- Principles of Medical Ethics – Familiarize yourself with the core principles such as autonomy, justice, beneficence, and non-maleficence, and understand how they guide decisions in healthcare.
- Legal and Moral Boundaries – Recognize the difference between legal obligations and ethical considerations, particularly in areas such as patient consent and rights.
- Emerging Issues – Stay informed about contemporary ethical dilemmas related to technology, genetics, environmental issues, and healthcare policy.
Study Tips for Effective Preparation
- Review Key Concepts – Revisit foundational ethical theories and principles regularly to ensure a strong grasp of essential knowledge.
- Practice with Scenarios – Work through hypothetical situations to hone your critical thinking and application skills.
- Engage in Discussions – Participating in study groups or discussions can help clarify complex concepts and broaden your perspective.
- Use Resources – Utilize textbooks, online resources, and academic papers to deepen your understanding and stay updated on current debates in ethics.
By focusing on these areas, you can approach your preparation with confidence, ready to tackle the challenges presented in ethical assessments and demonstrate your ability to think critically and apply ethical reasoning effectively.
Answering Ethical Assessments Effectively
Approaching ethical assessments with clarity and structured reasoning is crucial for success. The key to delivering strong responses lies in the ability to critically evaluate scenarios and apply relevant ethical frameworks. It’s not just about providing an answer but about demonstrating an understanding of the complexities surrounding each dilemma. To excel, one must focus on presenting clear, logical arguments while addressing all aspects of the problem at hand.
Effective Strategies for Responding
- Identify the Core Issue: Before diving into a response, clearly identify the central ethical dilemma presented in the scenario. Understanding what’s at stake allows for a more focused and precise answer.
- Apply Relevant Theories: Use well-established ethical theories to support your argument. Drawing from frameworks such as deontology, utilitarianism, or virtue ethics helps ground your response in established principles.
- Consider Multiple Perspectives: Ethical dilemmas often involve multiple viewpoints. Presenting a balanced analysis that considers different perspectives will strengthen your argument and demonstrate critical thinking.
- Justify Your Position: It’s not enough to simply state your position; you must justify it with logical reasoning and examples. This demonstrates a deeper understanding of the ethical implications of your response.
- Structure Your Answer: A well-organized response is easier to follow and more convincing. Start with an introduction, follow with your analysis and application of theories, and conclude with a clear, reasoned position.
Example Approach to a Scenario
| Step | Action | Explanation |
|---|---|---|
| 1 | Identify the Ethical Dilemma | Understand the core issue, such as patient autonomy versus beneficence in healthcare decision-making. |
| 2 | Analyze Different Perspectives | Consider the interests of the individual versus the needs of the wider community. |
| 3 | Apply Ethical Theories | For example, apply utilitarianism to argue for the greatest good, or deontological ethics to emphasize duty and rights. |
| 4 | Present Your Position | State your conclusion, supported by ethical reasoning and justifications. |
By following these steps and applying a methodical approach, you can effectively navigate complex ethical issues and present a clear, well-reasoned response that demonstrates your understanding of the subject matter. Remember, clarity and logical reasoning are your best tools in crafting persuasive arguments.