Key Questions for Microbiology Exam 3
Preparing for a comprehensive test in the field of life sciences requires a thorough understanding of various key concepts. The material often covers a wide range of topics, from the smallest microorganisms to complex biological processes that affect health and disease. Mastering these concepts is crucial for success in your upcoming evaluation.
Understanding the core principles that govern cellular functions, pathogen interactions, and immune responses will not only help in acing the assessment but also deepen your overall grasp of the subject. The content can be vast, but focusing on the most important aspects can make the preparation more manageable and efficient.
By reviewing common areas of focus, such as microbial life cycles, the body’s defense mechanisms, and techniques used for diagnosis and treatment, you can ensure a strong foundation. Take time to familiarize yourself with these areas to perform confidently when facing the challenges of the test.
Important Topics for Microbiology Exam 3
In any comprehensive assessment covering the study of living organisms, certain topics are consistently emphasized due to their fundamental importance. These key areas encompass the core principles that explain how organisms interact with each other and their environment, how diseases spread, and the various mechanisms of defense. Mastering these subjects is essential for a successful performance.
One critical area of focus involves understanding the structure and function of different types of pathogens. This knowledge is vital for distinguishing between bacteria, viruses, fungi, and parasites, as each group has distinct characteristics and impacts on the body. Additionally, a strong grasp of the immune system’s role in protecting the host from these invaders will provide a deeper insight into disease prevention and treatment strategies.
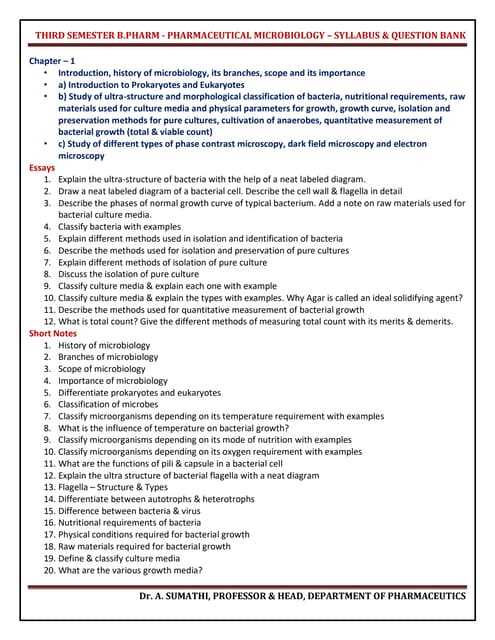
Another important subject is the methods used in laboratory diagnostics. Techniques for identifying pathogens and assessing their resistance to treatments are essential tools for medical professionals. Familiarity with these methods can enhance understanding and improve your ability to interpret various test results accurately.
Finally, studying microbial genetics and evolutionary processes is key. Understanding how microorganisms adapt, mutate, and evolve resistance mechanisms is crucial for addressing public health challenges, particularly in the context of antibiotic resistance and emerging infectious diseases.
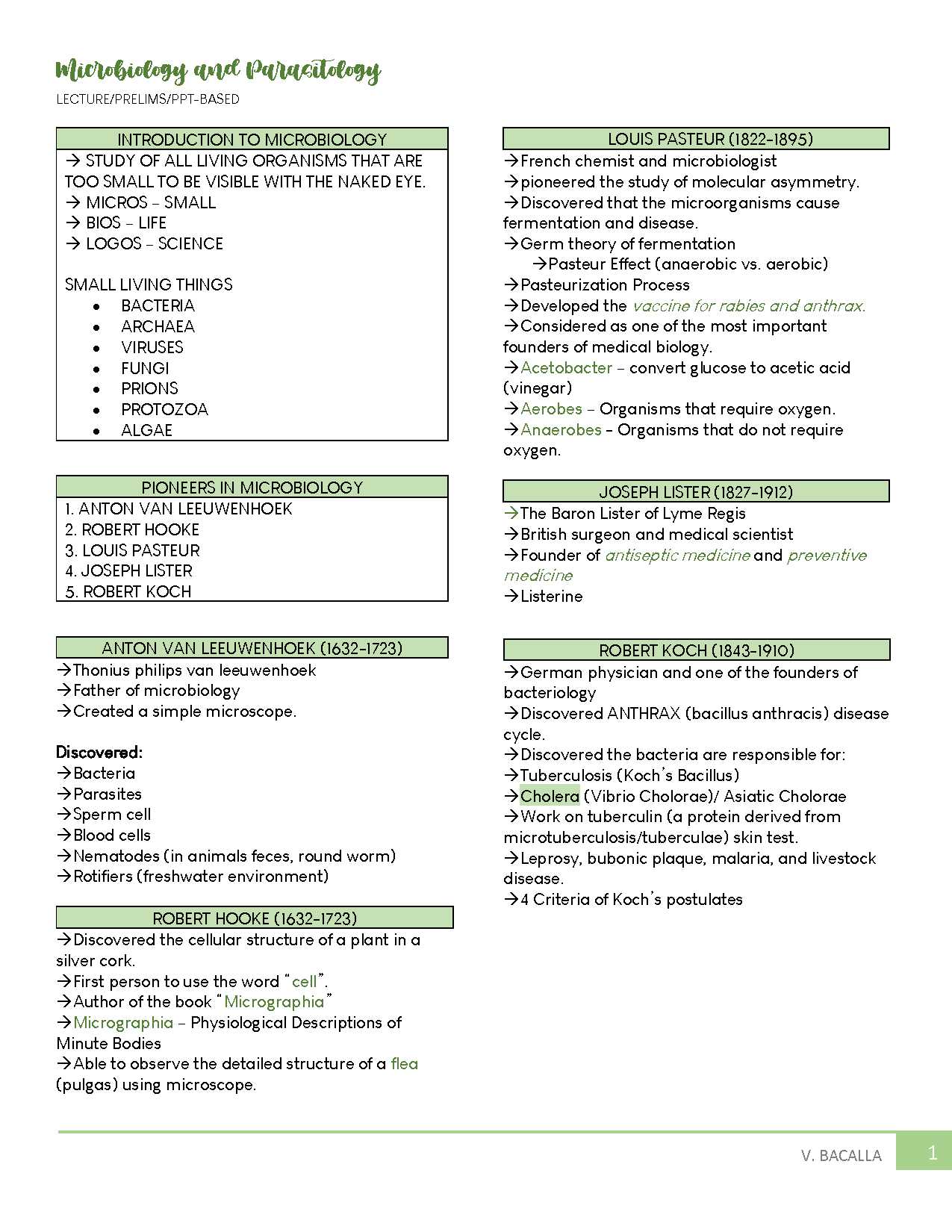
Understanding Key Microbial Pathogens
Studying harmful microorganisms is essential for understanding the mechanisms behind infections and diseases. These organisms, whether bacterial, viral, or fungal, play a significant role in human health. Recognizing their characteristics, behavior, and impact on the body can help in developing effective treatments and preventive strategies.
Bacterial Pathogens and Their Characteristics
Bacteria are among the most common culprits behind infectious diseases. These single-celled organisms can either thrive in the human body without causing harm or lead to serious health issues. Some bacteria produce toxins that damage tissues, while others might evade the immune system altogether. Understanding the different types of bacteria and their effects on human health is key to effective management.
Viruses and Their Mechanisms
Viruses operate differently from bacteria. They cannot replicate on their own and require a host cell to reproduce. Once inside a host, they hijack the cell’s machinery to make copies of themselves, often causing damage in the process. Some viruses can remain dormant for long periods, making them harder to detect and treat. Studying their behavior and transmission helps in developing vaccines and antiviral medications.
| Pathogen Type | Key Characteristics | Common Diseases |
|---|---|---|
| Bacteria | Single-celled, can be harmful or harmless, produce toxins | Pneumonia, Tuberculosis, Strep Throat |
| Viruses | Require host cell for replication, can be dormant | Flu, HIV, Hepatitis |
| Fungi | Multicellular, thrive in moist environments | Ringworm, Candida Infections |
Fungi, though not as commonly discussed as bacteria or viruses, can also cause significant harm, particularly in immunocompromised individuals. These organisms can infect skin, lungs, and other organs, often in environments where moisture and warmth are abundant. Understanding the variety of fungal infections is crucial for providing appropriate care.
Commonly Asked Questions in Microbiology Exams
Throughout any assessment focusing on the study of microorganisms, there are certain recurring themes and topics that are commonly tested. These areas are fundamental to understanding the interactions between microbes and their environments. Familiarity with these subjects helps in preparing for the challenges of such evaluations.
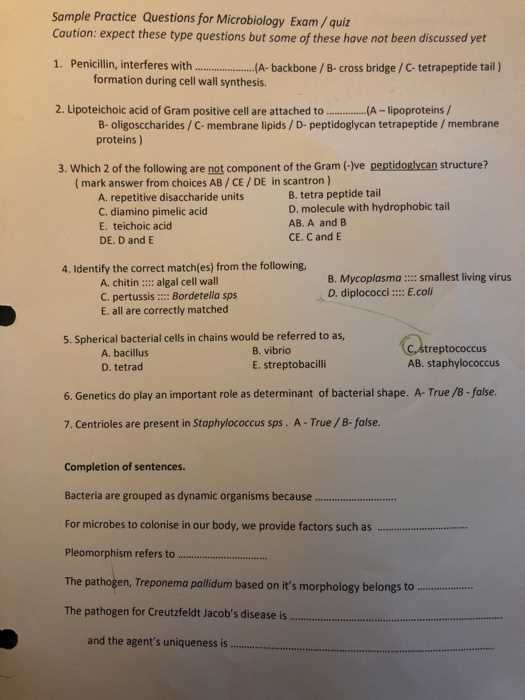
Understanding Pathogen Characteristics
One of the most common areas of focus is the distinction between different types of pathogens. Whether it is bacteria, viruses, fungi, or parasites, understanding the key features of these organisms, such as their structure, mode of reproduction, and how they cause disease, is crucial. Questions often revolve around identifying pathogens and explaining the symptoms associated with specific infections.
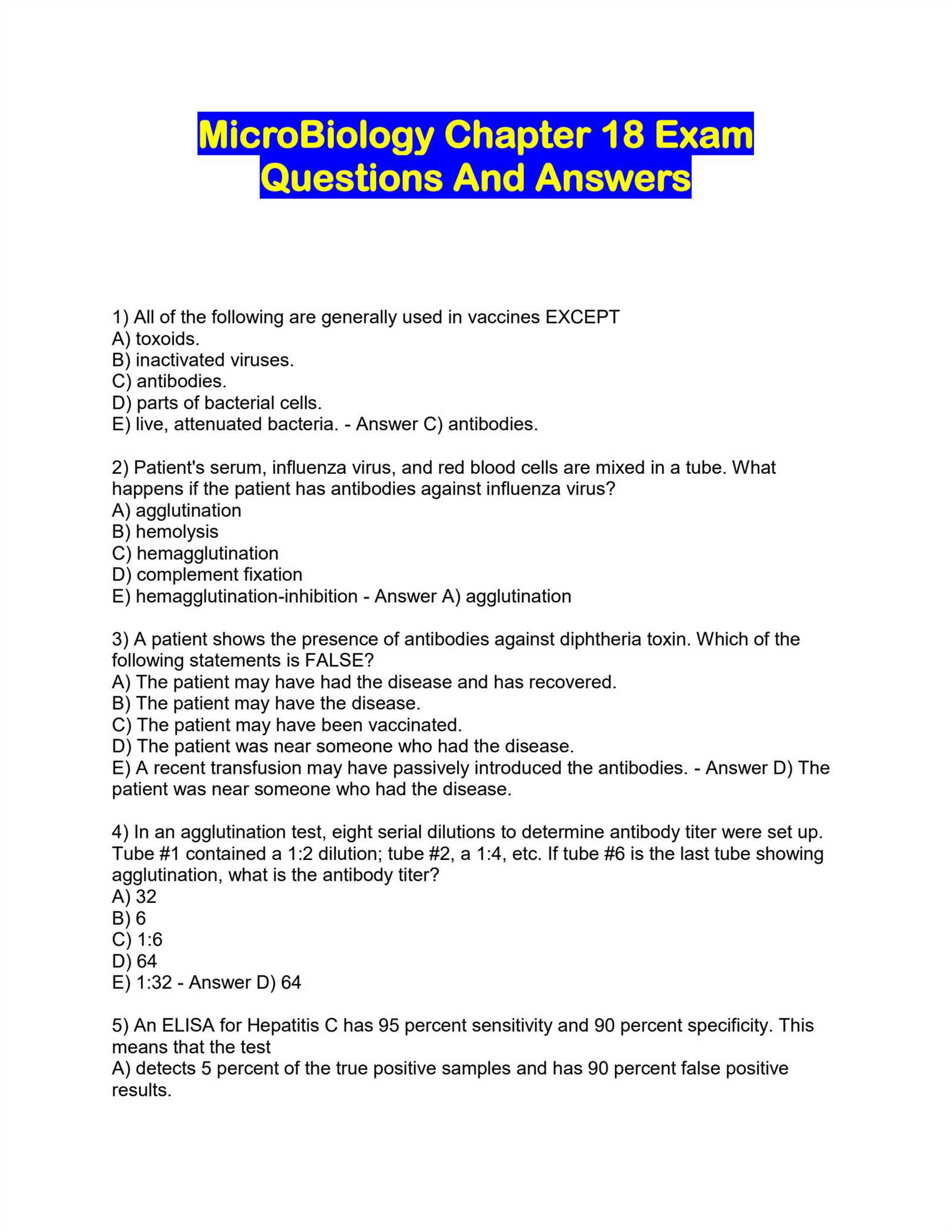
Immune System Responses and Mechanisms
The body’s response to harmful invaders is another critical topic. Expect questions that test your knowledge of the immune system, including the roles of different immune cells and the processes of inflammation, phagocytosis, and antibody production. Understanding how the body defends itself against infections, as well as the mechanisms pathogens use to evade the immune system, is often a central focus.
Additionally, questions may delve into how antimicrobial agents work, how pathogens develop resistance, and the implications of these resistance mechanisms on treatment strategies. Being well-versed in these topics allows for a deeper understanding of both the physiological and therapeutic aspects of infectious diseases.
How to Study Effectively for Exam 3
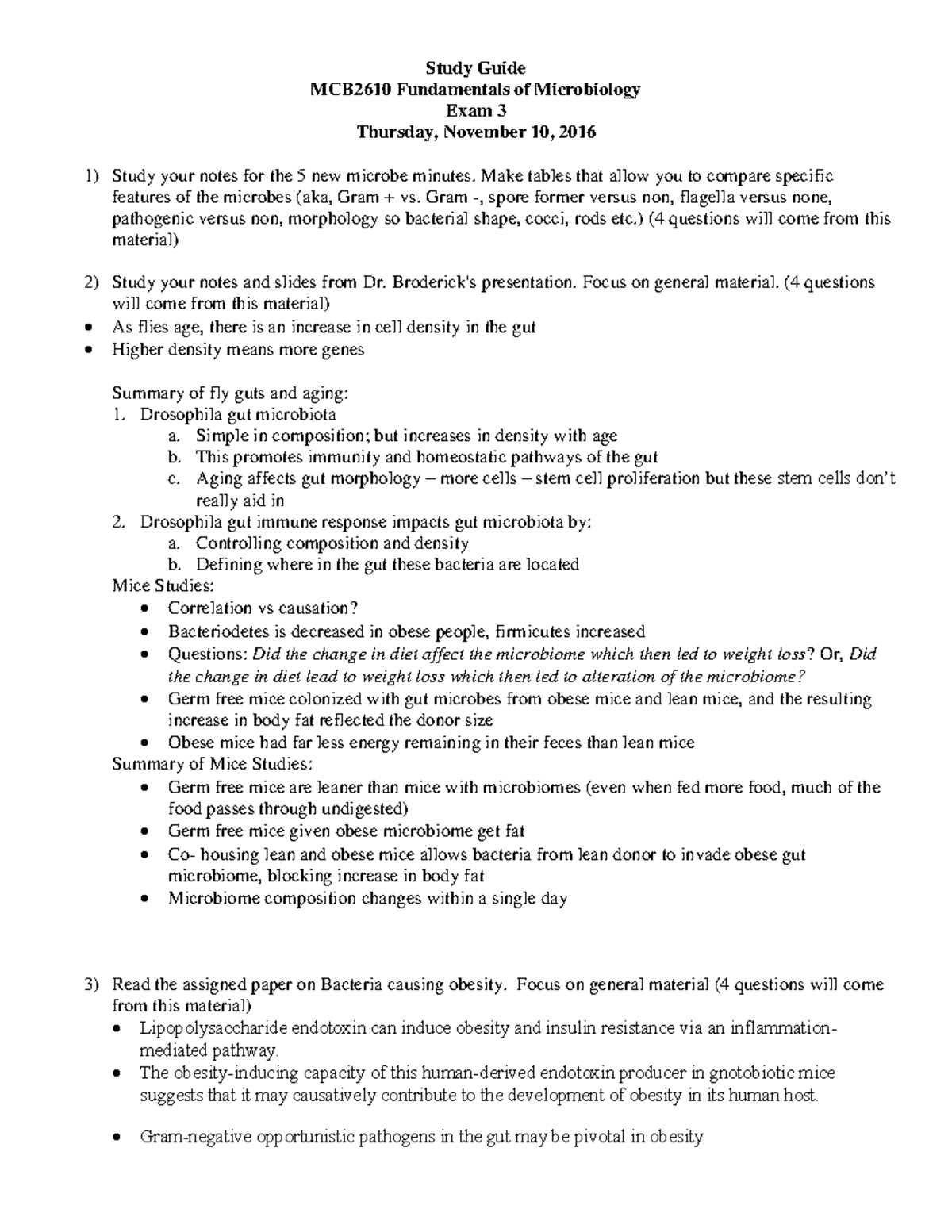
Preparing for a comprehensive test requires a structured and focused approach. To succeed, it is important to break down the material into manageable sections, prioritize key topics, and implement efficient study techniques. A well-organized study plan can greatly enhance your ability to retain information and perform confidently during the assessment.
Start by identifying the most important areas of study. Focus on the core concepts that are frequently covered in assessments, such as the characteristics of pathogens, the immune system’s defense mechanisms, and diagnostic techniques. Once you’ve highlighted these topics, create a study schedule that allocates time for each subject based on its level of importance and your familiarity with it.
Effective Study Techniques
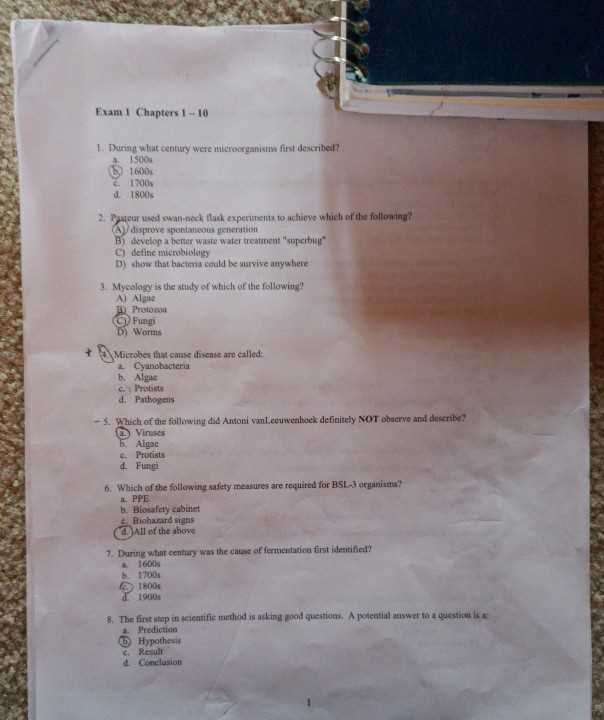
Use a combination of active learning strategies to reinforce your understanding. Flashcards, practice questions, and group discussions are all effective ways to engage with the material and test your knowledge. Regularly reviewing key concepts will help solidify your understanding and increase retention.
Review and Practice Regularly
Consistency is key when preparing for a challenging test. Set aside time each day to review material, even if it’s for a short period. The more frequently you revisit topics, the better you’ll internalize the information. Be sure to incorporate practical exercises, such as solving sample cases or explaining concepts out loud, to ensure you’re fully prepared.
| Study Method | Benefits |
|---|---|
| Flashcards | Improves recall and quick recognition |
| Group Discussions | Enhances understanding through collaboration |
| Practice Problems | Helps reinforce problem-solving skills |
By incorporating these methods into your routine, you’ll improve your preparation and be able to approach the assessment with confidence and clarity.
Exploring Microbial Growth and Reproduction
Understanding how microorganisms grow and reproduce is crucial for comprehending their life cycles and their potential impact on health. These tiny organisms can multiply rapidly under the right conditions, leading to either beneficial or harmful effects. The study of these processes provides essential insights into controlling infections and promoting the growth of beneficial microbes.
Microbial growth typically occurs through processes such as binary fission, where one cell divides into two identical cells. Environmental factors such as temperature, pH, and nutrient availability play a significant role in determining the rate of growth. By studying these conditions, we can predict how different types of microorganisms will behave in various environments.
Reproductive Methods in Microbes
While some microorganisms reproduce asexually through simple division, others may undergo more complex forms of reproduction, including spore formation and sexual reproduction. These methods ensure that the microorganisms adapt to changing environments, which can be vital for survival in hostile conditions.
Factors Influencing Growth Rates
The growth rate of microbes can be influenced by various external factors, including oxygen levels, nutrient types, and the presence of antimicrobial agents. Understanding these factors helps in designing effective control measures, particularly in medical or industrial applications where microbial growth needs to be regulated.
| Reproductive Method | Description |
|---|---|
| Binary Fission | Asexual reproduction where one cell divides into two identical cells |
| Spore Formation | Some microbes form spores to withstand adverse conditions |
| Sexual Reproduction | Involves the exchange of genetic material between two organisms |
By delving into these growth and reproductive mechanisms, researchers can better understand how to manage microbial populations and prevent harmful overgrowths, ensuring a balance between the natural world and human health.
Immune Response and Microbiology Concepts
The immune system plays a critical role in defending the body against harmful invaders such as pathogens. Understanding how the body responds to infections and the ways in which various microorganisms interact with the immune system is essential for grasping key concepts in this field. These mechanisms are fundamental not only for preventing disease but also for developing treatments and vaccines.
Defensive Mechanisms of the Immune System
The body has a sophisticated defense system designed to identify and eliminate harmful microorganisms. This system includes both innate and adaptive immunity. Innate immunity provides the first line of defense, using physical barriers like skin and mucous membranes, as well as specialized cells that recognize and attack invaders. On the other hand, adaptive immunity involves the creation of antibodies and memory cells that specifically target pathogens previously encountered.
Interactions Between Pathogens and the Immune System
Microorganisms have evolved various strategies to evade or overcome the immune system’s defenses. Some pathogens can mimic the body’s own cells, while others may produce substances that suppress immune responses. Understanding these interactions helps in designing effective therapeutic interventions, as well as in addressing issues like antibiotic resistance, which arises when pathogens become immune to treatment.
Antigen presentation and the activation of specific immune cells are crucial in determining how efficiently the immune system can eliminate harmful invaders. In-depth knowledge of these processes is vital for understanding how infections spread and how to combat them effectively.
Pathogenic Mechanisms and Disease Processes
Understanding how harmful agents interact with the host is key to exploring the development of illnesses. These agents employ various strategies to invade, damage, and evade the body’s defenses, leading to different disease manifestations.
- Entry Points: Pathogens often gain access through specific entry points like the respiratory tract, digestive system, or broken skin.
- Invasion Mechanisms: Once inside, these microorganisms may replicate and spread, disrupting normal body functions.
- Host Response: The body’s immune system reacts by activating defenses, though pathogens can sometimes resist these efforts.
- Tissue Damage: In some cases, the pathogen itself or the immune response causes harm to tissues, leading to inflammation or necrosis.
- Chronic Infection: Some pathogens may persist, causing long-term damage or recurring episodes of illness.
The balance between pathogen aggression and host defense determines the severity and progression of the disease, shaping clinical outcomes.
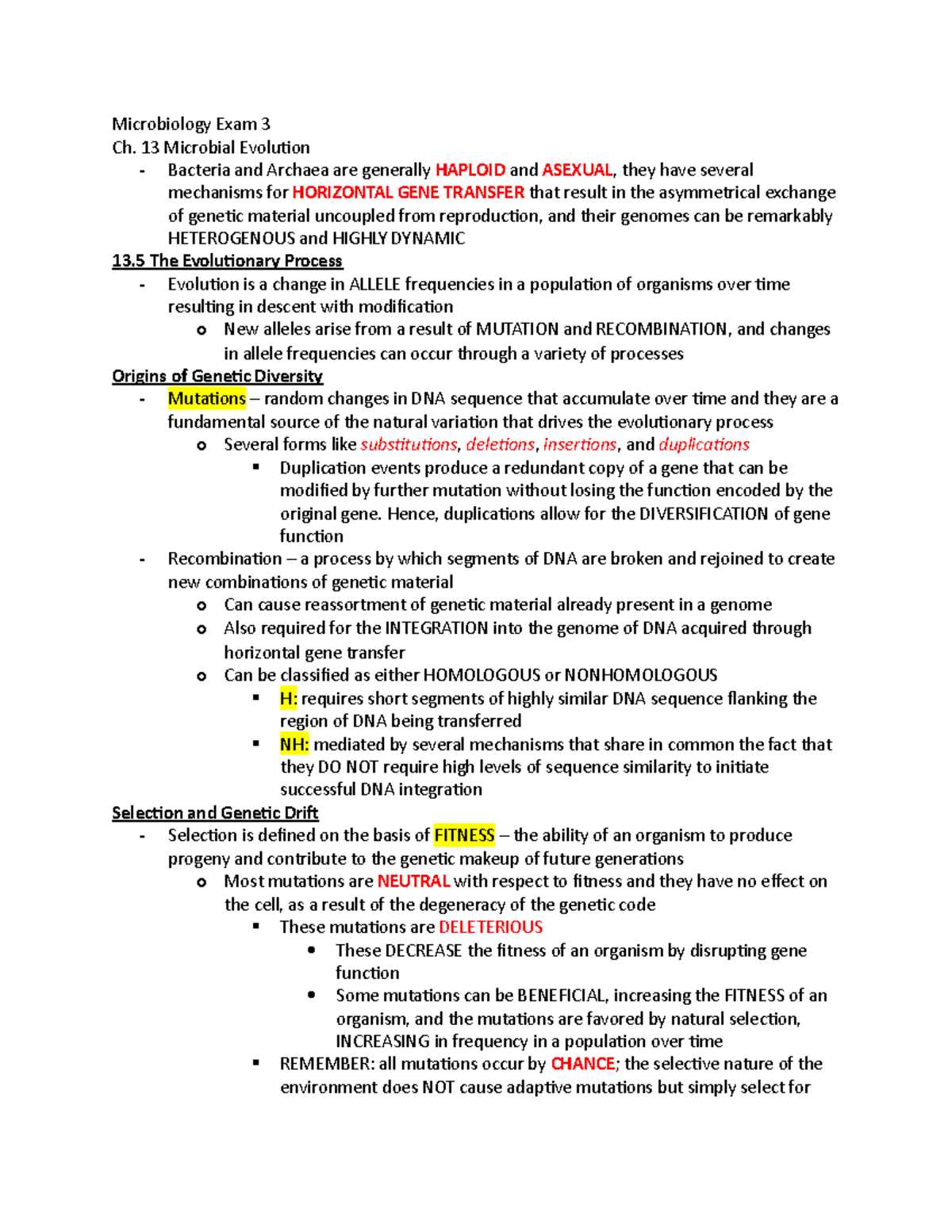
Microbial Genetics in Exam 3 Questions
Genetic material plays a central role in how microorganisms adapt, evolve, and cause disease. Understanding how genetic information is transferred, expressed, and modified in these organisms is essential to grasp their behavior and interactions with hosts.
Key Genetic Concepts
- Gene Transfer: Microbes can exchange genetic material through various mechanisms, such as transformation, transduction, and conjugation.
- Mutation: Changes in the genetic code can result in new traits, including resistance to drugs or increased virulence.
- Gene Regulation: The ability of microorganisms to turn genes on or off in response to environmental changes is crucial for survival and pathogenicity.
Applications and Importance
- Antibiotic Resistance: Genetic changes that confer resistance to antibiotics can spread rapidly, complicating treatment strategies.
- Virulence Factors: Specific genes contribute to the ability of pathogens to invade the host and cause disease.
- Biotechnological Advances: Understanding microbial genetics has led to breakthroughs in genetic engineering, vaccine development, and diagnostic techniques.
Important Bacterial Diseases to Know
Infectious diseases caused by bacteria are widespread and diverse, each affecting different systems within the body. Some of these illnesses are highly contagious, while others are more chronic or opportunistic, affecting individuals with weakened immune defenses. Understanding these diseases is essential to recognizing their symptoms, transmission methods, and treatments.
Common Bacterial Infections
- Tuberculosis: Caused by *Mycobacterium tuberculosis*, it primarily affects the lungs but can spread to other organs.
- Streptococcal Infections: Includes conditions like strep throat and pneumonia, caused by *Streptococcus* species.
- Cholera: A gastrointestinal infection caused by *Vibrio cholerae*, leading to severe diarrhea and dehydration.
- Typhoid Fever: Caused by *Salmonella typhi*, it can lead to high fever, abdominal pain, and other systemic symptoms.
- Leprosy: An infection by *Mycobacterium leprae*, which affects the skin, nerves, and mucous membranes.
Key Considerations and Management
- Antibiotic Resistance: Many bacterial diseases are becoming harder to treat due to increasing resistance to commonly used antibiotics.
- Prevention: Vaccination, hygiene practices, and safe food handling are crucial in preventing the spread of bacterial diseases.
- Early Diagnosis: Identifying bacterial infections early is important for effective treatment and to prevent complications.
Viruses and Viral Infections Overview
Viruses are unique infectious agents that rely on host cells to reproduce and propagate. Unlike bacteria, viruses do not have the machinery for independent life processes and can only replicate inside living cells. Their ability to infect various organisms, from humans to plants, makes them significant contributors to a wide range of diseases.
Viral infections can vary greatly in terms of severity and symptoms. Some viruses cause mild illnesses, while others can lead to chronic conditions or even death. These infections often spread rapidly through direct contact, air, or bodily fluids, complicating prevention and control efforts.
Understanding the life cycle of viruses, how they interact with host cells, and the immune system’s response is essential in managing and treating viral infections effectively.
Microbial Metabolism and Energy Production
Energy production is vital for the survival and growth of microorganisms. These organisms rely on various biochemical processes to convert nutrients into usable energy. Depending on environmental conditions and available resources, microbes can utilize different pathways to generate energy and support their cellular functions.
Key Metabolic Pathways
- Fermentation: An anaerobic process where organisms break down organic compounds, typically sugars, to produce energy and byproducts like alcohol or lactic acid.
- Aerobic Respiration: A process that requires oxygen to fully break down glucose and other molecules to produce a large amount of ATP (energy).
- Anaerobic Respiration: Similar to aerobic respiration but occurs in the absence of oxygen, using alternative electron acceptors like nitrate or sulfate.
- Photosynthesis: Some microbes, like cyanobacteria, use sunlight to produce energy, converting carbon dioxide and water into glucose and oxygen.
Energy Efficiency and Adaptation
- Energy Yield: Different metabolic pathways vary in efficiency, with aerobic respiration typically producing the most energy per molecule of glucose.
- Adaptation to Environment: Microbes can switch between different energy production pathways based on the availability of oxygen, nutrients, or light.
- Energy Conservation: In nutrient-poor environments, some microbes may slow down metabolic processes to conserve energy.
Fungi and Parasitic Infections
Fungal and parasitic infections are caused by organisms that can invade and affect various systems within the human body. While fungi are typically opportunistic pathogens, parasitic infections can range from mild to severe, depending on the species and the host’s immune response. These infections can lead to a variety of symptoms, often affecting the skin, gastrointestinal tract, or internal organs.
Fungal Infections
- Yeast Infections: Caused by *Candida* species, these infections often affect mucous membranes and skin, leading to conditions like thrush or vaginal infections.
- Dermatophyte Infections: Fungi such as *Trichophyton* cause superficial infections like ringworm, which affect the skin, nails, and hair.
- Systemic Fungal Infections: More severe conditions like histoplasmosis or cryptococcosis can spread to internal organs, particularly in immunocompromised individuals.
Parasitic Infections
- Protozoal Infections: Caused by single-celled organisms like *Plasmodium*, which causes malaria, and *Giardia*, which affects the gastrointestinal tract.
- Helminth Infections: Parasitic worms, such as roundworms or tapeworms, can infect various organs, leading to conditions like ascariasis or schistosomiasis.
- Ectoparasitic Infections: Organisms like lice or ticks infest the skin or hair and can transmit diseases like Lyme disease or typhus.
Both fungal and parasitic infections require specific treatments, and in many cases, prevention strategies such as hygiene and avoiding exposure are essential for reducing risk.
Diagnostic Techniques in Microbiology
Accurate diagnosis of infections caused by various pathogens is crucial for effective treatment. A wide range of methods are used to detect, identify, and analyze microorganisms. These techniques are essential for determining the cause of illness, guiding appropriate therapy, and preventing the spread of infectious diseases.
Traditional Diagnostic Methods
- Culture Techniques: Growing microorganisms on selective media allows identification based on colony characteristics, color, and shape.
- Microscopy: Staining techniques, such as Gram staining, enable visualization of microorganisms under the microscope, aiding in the identification of bacteria and fungi.
- Biochemical Tests: These tests help identify metabolic characteristics of pathogens, such as their ability to ferment sugars or produce specific enzymes.
Modern Diagnostic Approaches
- Polymerase Chain Reaction (PCR): A molecular method used to amplify and analyze genetic material, allowing for rapid and precise detection of pathogens.
- Serology: The detection of antibodies or antigens in blood samples can help identify recent or past infections.
- Immunofluorescence: A technique using fluorescently labeled antibodies to detect specific microorganisms or antigens in tissues or samples.
These diagnostic techniques are continuously evolving, improving both speed and accuracy, and enabling more personalized treatment plans for patients.
Laboratory Methods for Microbial Identification
Identifying microorganisms in the laboratory is a critical step in understanding infectious agents and determining appropriate treatments. Various methods are employed to accurately isolate and identify microbes, each with its strengths depending on the type of organism and the available resources.
Conventional Identification Techniques
- Culture Methods: Isolating microorganisms by growing them on selective media allows for observation of colony characteristics, helping to distinguish between different species.
- Staining Procedures: Techniques such as Gram staining or acid-fast staining are used to identify and classify microorganisms based on their cell wall structure and staining properties.
- Biochemical Testing: These tests assess the metabolic activity of microbes, such as their ability to ferment sugars or produce specific enzymes, aiding in species identification.
Molecular and Advanced Methods
- Polymerase Chain Reaction (PCR): This method amplifies specific DNA sequences, enabling precise identification of pathogens, even in small or mixed samples.
- Mass Spectrometry: Techniques like MALDI-TOF (Matrix-Assisted Laser Desorption/Ionization-Time of Flight) are used to analyze the molecular fingerprints of microbes for rapid identification.
- Gene Sequencing: Sequencing the genetic material of a microorganism provides detailed insights into its identity, strain variations, and relatedness to other species.
These laboratory methods are essential for accurately diagnosing infections, studying microbial diversity, and monitoring resistance patterns in clinical settings.
Reviewing Microbial Evolution and Ecology
Understanding the evolution and ecological roles of microorganisms is essential for grasping their impact on health, environment, and evolution. These organisms have adapted to an immense variety of habitats, developing unique survival strategies and contributing to the balance of ecosystems. Examining how they evolve and interact with their surroundings reveals important insights into their function and resilience.
Evolutionary Dynamics of Microbes
- Genetic Variation: Microbial populations evolve through mutations, horizontal gene transfer, and selective pressures, allowing them to adapt quickly to changing environments.
- Adaptation Mechanisms: Microbes develop resistance to antibiotics, form spores for survival in harsh conditions, or utilize novel metabolic pathways to thrive in diverse niches.
- Co-evolution with Hosts: Many microorganisms evolve in close interaction with their hosts, leading to complex relationships such as symbiosis or pathogenicity.
Ecological Interactions and Environmental Impact
- Microbial Communities: Microorganisms often exist in complex communities, such as biofilms, where they interact with each other and their environment to enhance survival and nutrient acquisition.
- Nutrient Cycling: Microbes play a critical role in recycling nutrients like nitrogen, carbon, and sulfur, facilitating ecosystem functions and supporting life on Earth.
- Environmental Adaptation: Microbial species can thrive in extreme conditions, such as high temperature, acidity, or salinity, expanding the boundaries of life.
By studying microbial evolution and ecology, we can better understand how these organisms influence the world around us and how they have shaped the development of life over billions of years.