Advanced Cardiovascular Life Support Exam C Answers
In the medical field, the ability to handle emergency situations with precision is essential. Whether you’re dealing with life-threatening conditions or ensuring that all protocols are followed correctly, mastering these skills is crucial for saving lives. The process of becoming proficient involves not only practical experience but also thorough testing to confirm your understanding of essential procedures.
The following section will guide you through the key areas of focus for those aiming to refine their knowledge and skills in urgent care scenarios. We’ll cover fundamental methods, highlight common challenges, and explore the necessary steps to prepare effectively for this vital certification.
By gaining a deep understanding of the critical steps involved, you’ll be better equipped to approach high-pressure situations confidently. Through comprehensive practice and review, you can enhance your ability to make quick, accurate decisions when every second counts.
Critical Care Procedures and Knowledge Verification
In emergency medical scenarios, ensuring that healthcare professionals can respond swiftly and accurately is paramount. A comprehensive understanding of critical procedures is necessary for managing high-stakes situations effectively. The process of verifying this knowledge is not just about answering questions, but about demonstrating competence in applying these techniques under pressure.
This section focuses on the key topics that are typically tested in high-pressure assessments for those in healthcare roles. Mastery of these principles will help in passing the required tests and solidifying your ability to make sound decisions in urgent situations. Here, we break down the essential concepts that are crucial for demonstrating your readiness and expertise.
Key Areas of Focus
Healthcare professionals must be familiar with a variety of scenarios and protocols, which are central to their training. The key concepts often include medication usage, response protocols, and resuscitation techniques. These elements form the foundation of the tests and ensure the individual’s ability to handle emergencies effectively.
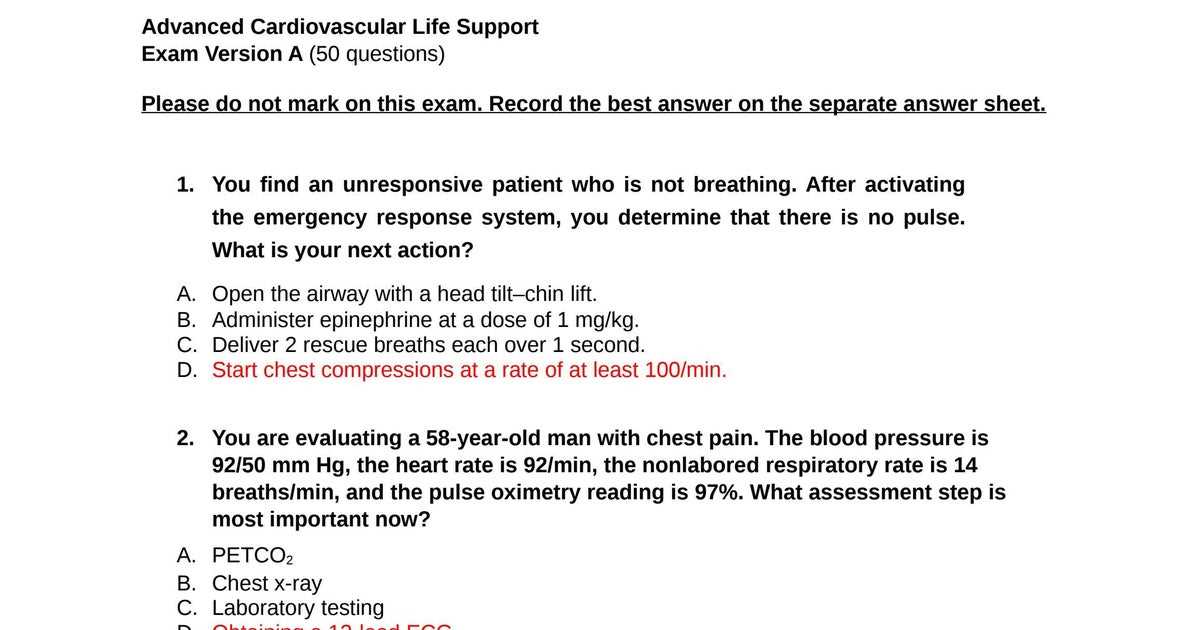
Test Question Examples
Below is a table that illustrates sample scenarios and questions that might appear in a high-stakes medical knowledge assessment. These examples represent the type of critical thinking required in real-world situations.
| Scenario | Correct Response | Rationale |
|---|---|---|
| Unresponsive patient with no pulse | Begin chest compressions immediately | Chest compressions are essential for maintaining circulation until further intervention is possible. |
| Patient exhibiting irregular heart rhythm | Administer appropriate anti-arrhythmic medication | Medications can help restore normal rhythm and stabilize the patient. |
| Patient with obstructed airway | Perform Heimlich maneuver | The Heimlich maneuver can remove the obstruction and restore normal breathing. |
Understanding these procedures and protocols is vital not only for passing assessments but for ensuring effective patient care during critical moments. The key is to focus on mastering each aspect and understanding its application in a real-world setting.
Understanding ACLS Exam C Structure
When preparing for high-stakes medical assessments, it’s important to understand the structure and content of the test. Knowing how the evaluation is organized helps you focus on the right areas and approach each section with confidence. These assessments typically cover a variety of critical skills that healthcare professionals need to perform under pressure, so familiarity with the format is essential.
Key Components of the Assessment
The structure of this test is designed to challenge your knowledge and ability to apply medical protocols in real-life emergency situations. It is divided into several distinct sections, each focusing on a different aspect of patient care. Here are some of the main categories:
- Protocol knowledge and understanding
- Decision-making under pressure
- Ability to interpret medical scenarios
- Practical application of techniques and procedures
- Drug administration and dosage calculations
Test Format and Question Types
The questions on this assessment are typically scenario-based, requiring you to choose the best course of action in a given situation. The format often includes:
- Multiple-choice questions with a focus on clinical decision-making
- Case studies that require detailed responses based on protocols
- True/false questions to test fundamental concepts
- Short answer or essay questions to assess critical thinking skills
By understanding the structure and types of questions you’ll face, you can better prepare yourself to tackle the challenges of this important certification. Each section tests a different skill, ensuring you are well-rounded and ready for any emergency situation that may arise.
Key Concepts in Critical Care Procedures
In critical care, the ability to act quickly and correctly can mean the difference between life and death. Understanding the core principles behind emergency protocols is essential for anyone involved in high-pressure medical situations. These fundamental concepts ensure that healthcare providers can respond effectively to patients in need of immediate attention.
Familiarity with the key procedures, medications, and decision-making processes is crucial. These elements guide practitioners through various emergencies, from heart attacks to respiratory distress, ensuring that each action taken is grounded in proven medical practices.
Key concepts include:
- Airway management – Ensuring that the patient’s airway is clear and that proper ventilation techniques are employed.
- Chest compressions – The cornerstone of resuscitation, used to maintain blood flow when the heart is unable to pump effectively.
- Defibrillation – The use of electrical shocks to reset the heart’s rhythm during certain types of arrhythmias.
- Medications – The proper use of drugs to stabilize the patient’s condition and correct underlying issues like arrhythmias.
- Rapid assessment – Quickly determining the severity of the situation and initiating the correct protocol.
Mastering these concepts ensures that healthcare providers can apply them under pressure, resulting in more effective patient outcomes. The goal is to be prepared for any situation and to act swiftly with confidence, using a structured approach to emergency care.
Preparing for ACLS Exam C Effectively
Successfully passing a critical care assessment requires more than just memorizing facts; it involves developing a deep understanding of key medical procedures and the ability to apply them in high-pressure situations. Preparing for the assessment means focusing on both theoretical knowledge and practical skills. With the right approach, you can ensure that you are well-prepared and confident for the test.
The preparation process should be systematic and targeted. Focus on mastering the most essential protocols, understanding the rationale behind each step, and practicing under timed conditions to simulate real-world scenarios. Here are some strategies to help you prepare effectively:
Study and Review Key Topics
To ensure you are fully prepared, dedicate time to studying the most important areas. These include:
- Patient assessment and recognition of critical conditions
- Emergency medication protocols and dosages
- CPR techniques and defibrillation methods
- Airway management and respiratory support
- Decision-making in time-sensitive situations
Practical Training and Simulation
While theoretical knowledge is vital, hands-on practice is equally important. Engage in simulation exercises to get comfortable with performing critical procedures under pressure. These can be done through:
- Mock drills with fellow healthcare providers
- Online practice tests and quizzes to assess your readiness
- Realistic scenario-based training to test decision-making skills
By incorporating both study and practice, you can reinforce your understanding of essential procedures and improve your ability to make quick, accurate decisions during an emergency.
Time Management Techniques
During the assessment, time management is crucial. Use these strategies to optimize your preparation:
- Set a study schedule with regular breaks to maintain focus
- Practice answering questions within a set time limit to build speed
- Review materials regularly to reinforce memory retention
Effective preparation involves mastering both the knowledge and the ability to respond quickly. With consistent effort and focus, you will be ready to handle any challenge the test presents.
Common Mistakes During ACLS Exam C
When preparing for a high-stakes medical assessment, it’s easy to fall into certain traps that can negatively impact performance. Common mistakes often arise from a lack of preparation, poor time management, or misunderstanding key concepts. Identifying these pitfalls ahead of time can help you avoid them and increase your chances of success.
Many candidates make errors due to stress or nervousness, which can cloud their judgment during critical decision-making. These mistakes can range from simple oversights to fundamental misunderstandings of essential procedures. Recognizing and addressing these issues during preparation is key to improving your performance.
Frequent Errors to Watch Out For
- Misinterpreting Scenarios – Failing to accurately assess the patient’s condition can lead to incorrect actions. Always focus on gathering all relevant information before making decisions.
- Poor Time Management – Rushing through questions or scenarios without considering all options can result in missed details or incorrect choices. Allocate time carefully and review your answers when possible.
- Skipping Key Protocols – Sometimes, candidates overlook critical steps in a protocol. Always follow the established guidelines step by step, even under pressure.
- Inconsistent Practice – Lack of regular, hands-on practice can cause hesitation when performing procedures. Engage in frequent simulation exercises to build confidence and speed.
- Overlooking Medication Dosages – In emergency situations, administering the wrong dosage or using an inappropriate drug can have serious consequences. Make sure you understand the correct dosages for various medications.
How to Avoid These Mistakes
By staying focused, practicing consistently, and reviewing key concepts, you can minimize errors. Consider these tips to strengthen your preparation:
- Review common protocols and decision-making processes regularly.
- Practice timed simulations to build confidence and speed.
- Stay calm under pressure by using deep-breathing techniques or relaxation exercises.
- Focus on accuracy first, then speed, when answering questions or performing tasks.
Being aware of these common mistakes and taking steps to prevent them will help you approach the assessment with confidence and improve your chances of success.
How to Interpret ACLS Exam Questions
Understanding how to approach questions on a critical care assessment is just as important as knowing the material itself. The way questions are structured can sometimes make it difficult to pinpoint the correct answer if not carefully analyzed. To succeed, you must learn how to read and interpret questions efficiently, ensuring you focus on the most important details that influence the right course of action.
Effective interpretation involves identifying key words, recognizing common scenario patterns, and applying your knowledge to make the best decision. Below are some strategies to help you navigate and answer questions accurately.
Breaking Down the Question
Each question is designed to assess your understanding of medical protocols and your ability to make the right decision quickly. Start by carefully reading the entire question to ensure you understand the situation before selecting your answer. Here are some tips for breaking down questions:
- Identify the key scenario – Focus on the main problem, such as a specific emergency situation or patient condition.
- Look for critical time-sensitive clues – Many questions will emphasize urgency, highlighting time frames for intervention.
- Notice any specific protocols mentioned – Recognize the medical procedures or drug interventions referenced in the question.
- Consider all options – Always review each choice carefully to determine which response fits the situation best.
Common Question Formats
Questions on this type of assessment typically follow certain formats. Familiarity with these can help you quickly understand the type of response needed. Some common formats include:
| Format | Description | Example |
|---|---|---|
| Scenario-based | Describes a patient situation where you must determine the correct action. | “A patient presents with sudden chest pain and shortness of breath. What is the first step in treatment?” |
| Procedure-based | Focuses on understanding the steps involved in a procedure or protocol. | “What is the next step after initiating chest compressions?” |
| Dosage and medication | Requires knowledge of correct drug dosages and administration procedures. | “What is the correct dosage for epinephrine in an adult patient during resuscitation?” |
Understanding these formats will help you read questions more effectively and choose the correct answers based on the scenario described. By practicing these strategies, you’ll be better prepared to navigate through the questions with confidence and clarity.
Essential Life-Saving Techniques for ACLS
When responding to a critical medical emergency, knowing and applying the right techniques is vital for improving patient outcomes. These life-saving interventions are designed to stabilize patients during severe situations, such as cardiac arrest, respiratory failure, or other life-threatening events. Mastery of these techniques is crucial for healthcare providers, as the ability to act quickly and accurately can save lives.
Each procedure or intervention serves a specific purpose, and understanding when and how to use them is essential. From clearing the airway to administering medications, these steps ensure the patient receives the best care possible in the critical moments following a medical emergency.
Key Techniques to Master
The following life-saving techniques are essential for any healthcare provider involved in emergency care:
- Chest Compressions – Effective chest compressions are fundamental in maintaining blood circulation during cardiac arrest.
- Defibrillation – The use of electrical shocks to restore a normal heart rhythm when the heart is experiencing arrhythmias.
- Airway Management – Ensuring the patient’s airway is open and clear to provide proper ventilation.
- Medication Administration – Correctly dosing and administering emergency medications to stabilize the patient’s condition.
- Rapid Assessment – Quickly assessing the patient’s condition to determine the most effective course of action.
Life-Saving Techniques in Action
Understanding these techniques in theory is one thing, but applying them effectively under pressure is another. Below is a table that highlights the most common scenarios and the corresponding life-saving technique:
| Scenario | Technique | Purpose |
|---|---|---|
| Cardiac Arrest | Chest Compressions & Defibrillation | To restore blood flow and correct abnormal heart rhythms |
| Respiratory Failure | Airway Management & Ventilation | To ensure the patient can breathe and receive adequate oxygen |
| Drug Overdose | Medication Administration | To counteract the effects of harmful substances and stabilize the patient |
| Shock | Fluid Resuscitation & Medications | To restore blood volume and improve circulation |
Mastering these essential techniques ensures that healthcare providers are prepared to act swiftly and effectively during emergencies. Through both practice and knowledge, you can improve patient outcomes in critical situations.
ACLS Algorithm Overview for Success
In high-pressure medical situations, having a clear, step-by-step guide can significantly improve outcomes. Algorithms are crucial tools that provide structured pathways for responding to emergencies, particularly when quick, decisive actions are required. Understanding and applying these protocols effectively is essential for achieving success in critical care scenarios.
These guidelines help healthcare providers make quick decisions, prioritize actions, and ensure all necessary steps are followed. Whether handling cardiac arrest, arrhythmias, or respiratory distress, the algorithms ensure that key procedures are performed systematically and efficiently.
Key Elements of the ACLS Algorithm
ACLS algorithms break down complex procedures into easy-to-follow steps, which guide medical professionals through each stage of a critical situation. Here are the key components you should understand:
- Initial Assessment – The first step is always assessing the patient’s condition. This includes checking responsiveness, breathing, and pulse.
- Airway Management – Ensuring the airway is open is critical to proper ventilation and oxygenation.
- Cardiac Arrest Management – In cases of cardiac arrest, algorithms prioritize chest compressions and defibrillation, followed by the administration of emergency medications.
- Arrhythmia Protocol – Different types of arrhythmias require different interventions, such as synchronized cardioversion or antiarrhythmic medications.
- Post-Resuscitation Care – After stabilization, algorithms guide the steps for ongoing care, including temperature management and monitoring.
Applying the ACLS Algorithm in Practice
To effectively apply these algorithms, healthcare providers must become familiar with their structure and logic. Here’s how the process typically unfolds in a real-world scenario:
- Start with a quick initial assessment of the patient’s airway, breathing, and circulation.
- Begin chest compressions immediately if there is no pulse, followed by defibrillation if indicated.
- Administer medications as required based on the identified arrhythmia or cause of collapse.
- Continue advanced interventions while monitoring the patient’s response and adjusting the care as needed.
- Once the patient is stabilized, shift focus to post-resuscitation care to prevent further complications.
Mastering the use of these algorithms ensures that healthcare providers can perform life-saving interventions in a systematic and organized manner. Familiarity with these steps is a key factor in improving patient survival rates and achieving optimal outcomes in emergency care.
Understanding Cardiac Arrest Treatment Protocols
When a person experiences a cardiac arrest, immediate and precise treatment is critical to restoring normal heart function and ensuring survival. Treatment protocols are established guidelines that outline the essential steps in responding to this life-threatening event. These protocols are designed to help healthcare providers make quick, informed decisions in high-pressure situations, maximizing the chances of successful resuscitation.
Understanding these protocols is vital for anyone involved in emergency care, as each step is focused on stabilizing the patient and addressing the root causes of cardiac arrest. The key to success lies in the swift execution of these interventions, which include assessing the patient, performing chest compressions, and using defibrillation when necessary.
Core Elements of Cardiac Arrest Protocols
The treatment for cardiac arrest follows a structured approach to ensure no step is overlooked. The following elements form the foundation of these protocols:
- Initial Assessment – Quickly determining the patient’s condition by checking for responsiveness, breathing, and pulse is the first crucial step.
- Chest Compressions – High-quality chest compressions are the cornerstone of cardiac arrest management, ensuring blood flow to vital organs until further intervention can be made.
- Defibrillation – In cases of certain arrhythmias, an electric shock (defibrillation) may be necessary to restore normal heart rhythm.
- Medication Administration – Drugs may be used to stabilize heart rhythm or improve blood pressure, depending on the underlying cause of the arrest.
- Post-Resuscitation Care – Once the patient is revived, ongoing care such as temperature regulation and monitoring is essential to prevent further complications.
Step-by-Step Protocol for Cardiac Arrest Management
Following a clear and systematic approach is essential for providing the best chance of recovery. Below is an overview of the typical steps involved in treating cardiac arrest:
- Assess the patient’s condition immediately. Check for a pulse, breathing, and responsiveness. If absent, begin chest compressions.
- Call for emergency help and activate the advanced care team if needed. Defibrillation may be indicated depending on the rhythm detected.
- Continue chest compressions while awaiting a defibrillator. If available, administer shocks according to the guidelines for shockable rhythms.
- If defibrillation is unsuccessful or the rhythm is non-shockable, proceed with administering medications like epinephrine to help restore circulation.
- Once the patient is stabilized, transfer to post-resuscitation care, including monitoring vital signs and providing therapeutic interventions as necessary.
These treatment protocols ensure that every healthcare provider involved in cardiac arrest management is equipped to act quickly and efficiently. By understanding and applying these guidelines, medical professionals can dramatically improve the chances of survival for patients experiencing cardiac arrest.
Role of Medications in ACLS Protocols
In critical care situations, medications are a vital part of the treatment strategy for restoring a patient’s health and stabilizing their condition. Whether managing a heart attack, arrhythmia, or other life-threatening events, drugs are used to support the body’s functions, manage symptoms, and improve outcomes. Proper use of these medications can significantly enhance the effectiveness of interventions in emergency settings.
During resuscitation, the right medications are administered at the right time to address specific conditions. The goal is to restore normal heart rhythms, improve circulation, and optimize overall organ function. Medications can also help reduce the severity of the event, stabilize blood pressure, and prevent further complications.
Key Medications Used in Critical Care Protocols
- Vasopressors – Drugs like epinephrine and norepinephrine are used to constrict blood vessels and raise blood pressure, ensuring adequate perfusion of vital organs during cardiac arrest or shock.
- Antiarrhythmic Medications – Medications such as amiodarone and lidocaine are used to manage abnormal heart rhythms, helping to restore normal cardiac function.
- Defibrillation Agents – In cases of life-threatening arrhythmias like ventricular fibrillation, defibrillation agents like magnesium sulfate may be administered to improve the chances of successful defibrillation.
- Fluid Resuscitation – IV fluids are used to restore circulating blood volume, helping to stabilize blood pressure and improve organ perfusion.
- Analgesics and Sedatives – In some critical care situations, medications for pain relief and sedation may be necessary to reduce discomfort and manage the patient’s anxiety or agitation during treatment.
Proper Administration and Timing of Medications
One of the key factors in the success of treatment protocols is the timely and accurate administration of medications. Here’s how they are typically used in emergency care:
- Early Intervention – Certain medications, such as epinephrine, are given immediately after cardiac arrest to help restore circulation and improve the chances of resuscitation.
- Rhythm Control – Antiarrhythmic drugs are administered based on the type of arrhythmia detected, helping to correct abnormal heart rhythms and prevent complications.
- Fluid Management – IV fluids are given to maintain adequate circulation, especially in cases where shock or hypovolemia is present.
- Post-Resuscitation Care – Following initial stabilization, additional medications may be required for ongoing management, including pain relief, sedation, or further treatment of underlying conditions.
Medications are essential tools in emergency care, providing the necessary support to help patients recover and prevent further harm. When administered correctly, they play a crucial role in improving outcomes for patients in critical conditions.
How to Manage Airway and Breathing in ACLS
Effective airway management and proper ventilation are critical components in stabilizing patients during medical emergencies. Ensuring that the patient is receiving adequate oxygenation can greatly impact the outcome, especially in cases of cardiac arrest, respiratory failure, or other life-threatening conditions. Proper techniques and timely interventions can prevent further complications and improve chances of recovery.
When managing the airway, it is important to secure a clear and open pathway for air to flow into the lungs. This often involves using specific equipment, such as endotracheal tubes, airway adjuncts, and ventilation devices. Ensuring that the patient’s breathing is sufficient and effective helps prevent hypoxia, a condition where the body is deprived of necessary oxygen, which can lead to organ damage and other severe complications.
Airway Management Techniques
Proper airway management is essential in any critical care scenario. Some common techniques and tools include:
- Head-Tilt Chin-Lift – A basic maneuver to open the airway by tilting the head back and lifting the chin to clear any obstructions.
- Oropharyngeal and Nasopharyngeal Airways – Devices used to maintain an open airway, especially in patients who are unconscious or unresponsive.
- Endotracheal Intubation – A more advanced method of securing the airway, involving the insertion of a tube into the trachea to ensure adequate oxygen delivery.
- Supraglottic Airway Devices – Alternative devices, such as the Laryngeal Mask Airway (LMA), used when intubation is difficult or inappropriate.
Ventilation and Oxygenation
Once the airway is secured, ensuring proper ventilation and oxygenation is the next step in managing a patient’s breathing. This involves providing sufficient oxygen to the lungs to maintain normal oxygen levels in the blood. Common techniques include:
- Bag-Valve Mask (BVM) Ventilation – A technique used to provide manual ventilation, using a bag connected to a mask that covers the patient’s nose and mouth.
- Mechanical Ventilation – In cases where manual ventilation is not sufficient, mechanical ventilators may be used to provide controlled, continuous airflow to the lungs.
- Supplemental Oxygen – Administering oxygen via nasal cannula or face mask to ensure the patient is receiving an adequate supply of oxygen during treatment.
- Capnography – Monitoring the patient’s exhaled carbon dioxide to assess the effectiveness of ventilation and confirm proper tube placement during intubation.
By employing these techniques, healthcare providers can maintain the patient’s oxygenation and prevent further complications. Prompt and correct management of airway and breathing plays a pivotal role in patient recovery and is critical in the success of resuscitation efforts.
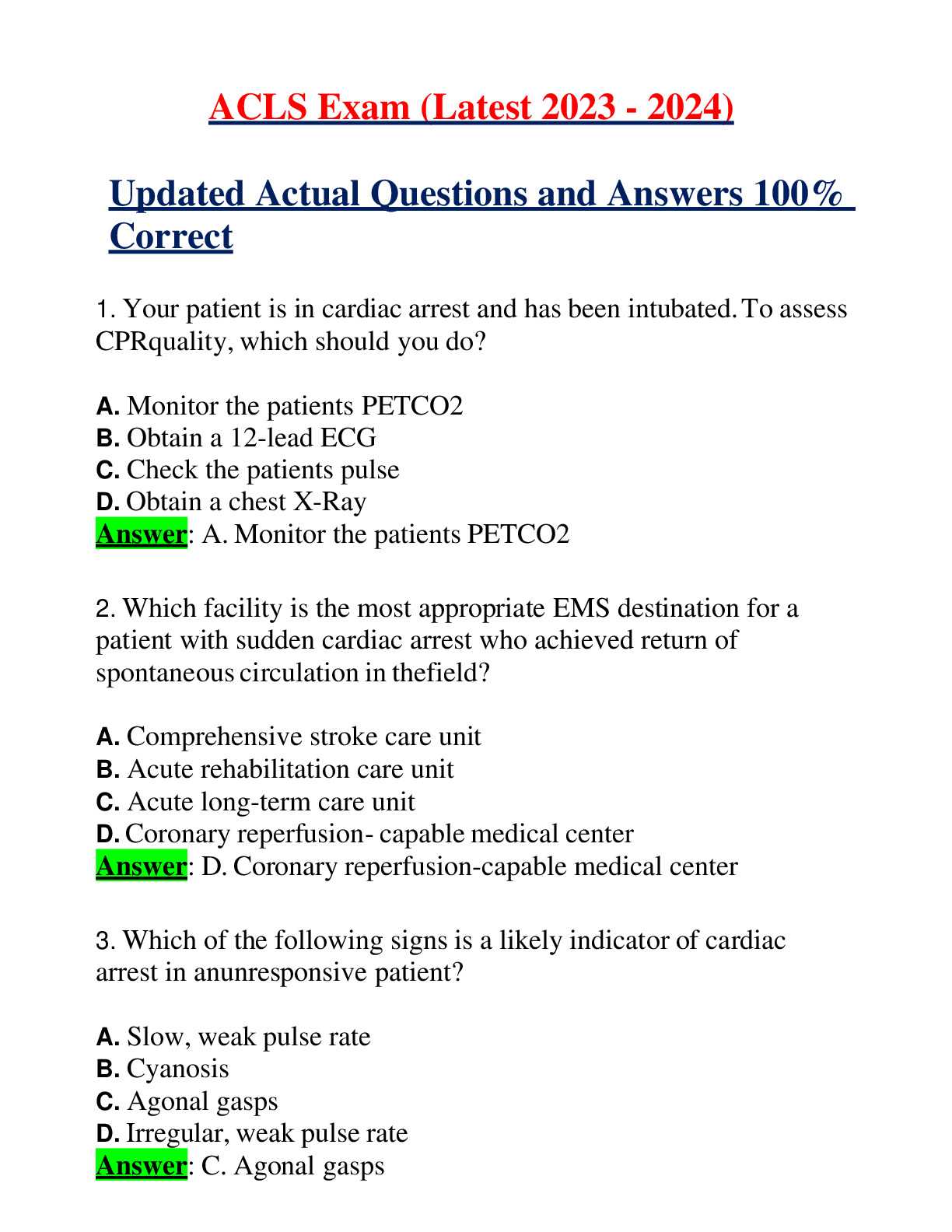
ACLS Practice Questions and Answers
Preparing for certification and proficiency assessments in critical care involves understanding key concepts through practice. Engaging with a variety of questions can help solidify knowledge, improve decision-making skills, and prepare you for real-world scenarios. Practice questions allow individuals to apply what they’ve learned in a simulated environment, helping to test their readiness and refine their skills.
By reviewing these questions and their corresponding explanations, you can gain a deeper insight into the protocols, procedures, and techniques used during emergency interventions. This method not only helps with memorization but also enhances your ability to think critically under pressure and make the right decisions in a time-sensitive setting.
Below is a selection of practice questions designed to challenge and assess your understanding of key concepts, as well as the correct methods to handle different emergency situations.
Sample Question 1
Question: A 65-year-old male presents with chest pain and shortness of breath. His heart rate is 120 beats per minute, and his blood pressure is 90/60 mmHg. What is the first intervention that should be performed?
- A) Administer aspirin
- B) Establish intravenous access
- C) Provide high-flow oxygen
- D) Begin chest compressions
Correct Answer: C) Provide high-flow oxygen. Immediate oxygen therapy should be given to improve oxygenation and prevent further cardiac or respiratory complications.
Sample Question 2
Question: A patient is in respiratory arrest with no pulse. What is the correct first step in the management of this patient?
- A) Check the airway and begin ventilation
- B) Administer epinephrine
- C) Perform chest compressions
- D) Prepare for defibrillation
Correct Answer: C) Perform chest compressions. The first step in treating a patient in cardiac arrest is high-quality chest compressions to maintain circulation until advanced interventions can be administered.
By regularly practicing these types of questions, individuals can enhance their knowledge and boost their confidence before facing critical scenarios. Familiarizing yourself with both the correct responses and rationales will increase your preparedness, ensuring you are ready for real-life situations.
Advanced Resuscitation Techniques for ACLS
Effective resuscitation in critical care situations requires a combination of techniques that ensure the best possible outcomes for patients in severe distress. The process involves systematic approaches to manage life-threatening conditions, restore circulation, and stabilize the patient. This section covers the most vital and advanced procedures that medical professionals rely on during emergencies, from cardiac arrest to respiratory failure.
Mastering these techniques is essential for healthcare providers involved in critical care, as they form the foundation for successful patient recovery and survival. By incorporating these strategies, teams can improve their ability to respond efficiently in time-sensitive situations and ensure they deliver high-quality care under pressure.
Chest Compression Techniques
High-quality chest compressions are critical in maintaining circulation during cardiac arrest. The primary goal is to generate sufficient blood flow to vital organs, especially the brain and heart, until more advanced interventions can be applied. Key considerations for effective chest compressions include:
- Depth: Compress the chest at least 2 inches (5 cm) deep.
- Rate: Maintain a compression rate of 100-120 per minute.
- Full recoil: Allow the chest to fully rise between compressions to ensure proper blood flow.
- Minimize interruptions: Limit pauses in chest compressions to under 10 seconds.
Defibrillation and Shock Delivery
Defibrillation is another critical component of advanced resuscitation techniques. It involves delivering a controlled electrical shock to the heart to restore a normal rhythm in cases of life-threatening arrhythmias such as ventricular fibrillation or pulseless ventricular tachycardia. The following steps are essential:
- Assess the patient’s rhythm using an ECG monitor.
- If the rhythm is shockable, deliver a defibrillation shock as per protocol.
- Ensure adequate chest compressions and oxygenation between shocks.
- Consider using an automated external defibrillator (AED) if available for faster response times.
Mastering these resuscitation techniques and performing them in a timely, effective manner can drastically improve survival rates in emergency situations. Regular practice and ongoing education in these methods are key to maintaining proficiency and delivering optimal patient care.
Critical Thinking in ACLS Exam C
Effective decision-making during emergency care situations often relies on the ability to think critically. In high-pressure scenarios, clinicians must evaluate complex data quickly and make informed choices that can directly impact patient outcomes. This section focuses on the importance of critical thinking in handling challenging situations, ensuring that healthcare providers respond appropriately to rapidly changing conditions.
Critical thinking involves more than just recalling protocols–it requires the ability to assess a patient’s condition, consider all available options, and prioritize actions based on the severity of the situation. By honing these skills, healthcare professionals can improve their decision-making process, reducing the likelihood of errors and increasing the chances of successful intervention.
During this process, it is important to consider the following elements:
- Recognizing key clinical signs and symptoms quickly.
- Evaluating available information such as heart rhythm, oxygen levels, and patient response.
- Anticipating complications and preparing for potential changes in the patient’s condition.
- Applying the most effective intervention based on current evidence and guidelines.
By actively engaging in critical thinking, healthcare providers ensure that they are not only following established guidelines but also tailoring their interventions to meet the specific needs of each patient. This skill is vital for effective management during emergencies, where time is limited, and every decision counts.
ACLS Exam C Scoring and Passing Criteria
When preparing for an emergency care certification assessment, understanding the scoring system and the requirements for passing is crucial. The evaluation process typically includes multiple-choice questions designed to assess knowledge of treatment protocols, patient management, and critical decision-making. This section will explain how the scoring is structured and outline the criteria for successfully completing the test.
Scoring Breakdown
The scoring for this assessment is based on the accuracy of answers, with each correct response contributing to the overall score. A specific passing threshold must be met to demonstrate a sufficient understanding of emergency response protocols. Here’s how the scoring typically works:
| Section | Points | Maximum Score |
|---|---|---|
| Knowledge Questions | 1 point per question | 100 points |
| Practical Scenarios | Varies depending on the scenario | 50 points |
| Total Possible Score | 150 points |
Passing Criteria
To pass the assessment, candidates typically need to achieve a minimum score, which ensures they have a solid grasp of essential procedures and patient care strategies. Although the exact passing score may vary, the general requirement is often around 80% or higher. Additionally, practical scenarios and situational questions are weighted heavily, emphasizing the importance of applying knowledge in real-world scenarios.
Once the test is completed, the results will indicate whether the candidate has successfully met the required standards. If a candidate does not pass on the first attempt, most programs offer opportunities for retaking the test, allowing individuals to review areas of weakness and improve their understanding before trying again.
Tips for Reviewing ACLS Exam Materials
When preparing for a certification test in critical care response, thorough review of the necessary materials is essential. A structured approach can enhance understanding and retention of the key concepts required for success. This section provides effective strategies to help focus your review efforts and ensure you are well-prepared for the assessment.
Effective Study Strategies
To maximize your review time, consider the following strategies:
- Focus on Core Protocols: Prioritize studying the primary treatment algorithms and decision-making protocols that are central to the assessment. These are often the most heavily tested areas.
- Utilize Practice Scenarios: Engage with case studies and situational questions that simulate real-world emergencies. These will help reinforce your practical understanding of procedures.
- Use Flashcards: Flashcards can be an effective tool for memorizing important terms, drugs, and protocols. They are also easy to review in short bursts.
- Review Guidelines Regularly: Continual review of the latest medical guidelines and best practices ensures that you are up to date with the most current approaches to emergency care.
- Test Yourself: Practice with mock questions or previous tests to familiarize yourself with the format and types of questions you may encounter.
Maximizing Retention
To help retain key information and improve recall during the test, consider these tips:
- Break Down Information: Break study sessions into smaller, manageable segments and focus on one topic at a time to prevent feeling overwhelmed.
- Teach What You’ve Learned: Explaining concepts to others can reinforce your understanding and help identify any areas that need more review.
- Rest and Revisit: Take regular breaks to avoid fatigue. Revisit the material periodically to keep it fresh in your mind.
By following these strategies, you can optimize your study time and increase your confidence, leading to better performance in the certification assessment.
Strategies for Time Management in ACLS Exam
Time management is a crucial skill when preparing for and taking high-stakes medical certification tests. With the wide range of concepts and protocols to master, balancing the depth of knowledge with the time available for each section is essential. This section offers practical tips for efficiently using your time throughout the preparation and the actual test-taking process.
Effective Preparation Techniques
Proper planning during your study sessions can help you avoid last-minute cramming and ensure you are well-prepared:
- Create a Study Schedule: Set aside specific times each day or week dedicated to review. Break down the material into smaller topics and assign realistic goals for each session.
- Prioritize Key Topics: Focus on the most critical protocols and algorithms that are frequently tested. Use practice questions to identify weaker areas and allocate more time to them.
- Practice Time-Limited Quizzes: Engage with practice tests that simulate the time constraints of the real assessment. This will help you improve your speed and familiarity with the test format.
- Avoid Overloading: Study in manageable blocks of time, taking regular breaks to maintain focus and avoid burnout.
Managing Time During the Test
Once you are in the testing environment, managing your time effectively can make a significant difference in your performance:
- Read Questions Carefully: Take a moment to thoroughly read each question to ensure you understand what is being asked before answering. Misunderstanding a question can cost valuable time.
- Allocate Time for Each Section: Divide your available time by sections and try to stick to the limits. If you’re spending too long on one question, move on and come back to it later.
- Skip and Return: If you get stuck on a question, skip it and move forward. You can always return to challenging questions once you’ve answered others, helping prevent unnecessary delays.
- Stay Calm and Focused: Managing anxiety during the test is key. Staying calm will help you think more clearly and manage your time more effectively.
By mastering these time-management strategies, you can ensure that you maximize your chances of success, both during the preparation phase and the actual assessment.
How to Retake the ACLS Exam C
If you haven’t passed the assessment yet, retaking it can seem daunting. However, with the right preparation and a strategic approach, you can increase your chances of success on the next attempt. This section provides guidance on how to effectively retake the test and improve your results.
Understanding the Retake Process
The process of retaking the assessment is straightforward, but it’s important to follow the guidelines set by the certification organization. Most programs allow you to retake the assessment after a set waiting period, which provides ample time for additional study and review.
- Check the Retake Policy: Review the policy of the organization offering the test. Many programs allow a retake within a specified time frame, but they may require you to pay a fee or complete additional review before attempting again.
- Review Your Results: If possible, review the areas where you struggled. Some programs provide feedback on incorrect answers, which can help you identify weak points to focus on.
- Sign Up for Retake: After confirming eligibility and addressing any gaps in knowledge, register for the retake by following the organization’s instructions.
Effective Strategies for Improvement
Once you’ve registered for the retake, it’s essential to prepare effectively. Consider the following strategies to improve your chances:
- Focus on Weak Areas: Identify the sections where you struggled in your previous attempt and spend extra time mastering those topics. Practice using mock tests to strengthen these areas.
- Review Key Protocols and Procedures: Make sure you are well-versed in the most critical concepts and protocols that are likely to be tested. This includes understanding the steps for emergency interventions and proper medication administration.
- Seek Additional Support: If you’re struggling with certain concepts, consider enrolling in a refresher course, seeking help from peers, or working with a mentor.
- Practice Under Test Conditions: Simulate exam conditions by taking practice tests with time limits. This will help you manage time effectively and become more familiar with the test’s format.
With focused effort and strategic preparation, you can improve your performance and successfully pass the retake, ensuring that you are fully equipped to handle critical situations when they arise.