Complete Guide to Newborn Physical Exam Write Up

Accurate documentation of an infant’s health assessment is crucial for monitoring their growth, development, and overall well-being. A thorough record helps healthcare providers track important milestones and identify potential issues early on. Clear and precise notes ensure that the information is easily accessible for future consultations and decision-making.
In this article, we will explore essential tips and methods for documenting the key aspects of an infant’s initial health evaluation. From the early stages of assessment to the interpretation of findings, each part of the process plays a significant role in delivering quality care. The goal is to provide practical guidance on how to approach the task of recording health data while ensuring accuracy and completeness.
By following best practices and understanding the importance of each detail, healthcare professionals can ensure they create reliable documentation that supports both their clinical decisions and the infant’s long-term health. Whether you’re a student, resident, or experienced practitioner, mastering the art of thorough documentation is an invaluable skill in any medical setting.
Newborn Health Assessment Documentation Guide
Documenting an infant’s health evaluation requires attention to detail and a structured approach to capture all relevant information. This process ensures that healthcare professionals can accurately track the baby’s progress, identify any concerns early, and communicate findings clearly with other members of the healthcare team. Proper documentation supports clinical decision-making and provides a foundation for future care plans.
Key Steps for Effective Documentation
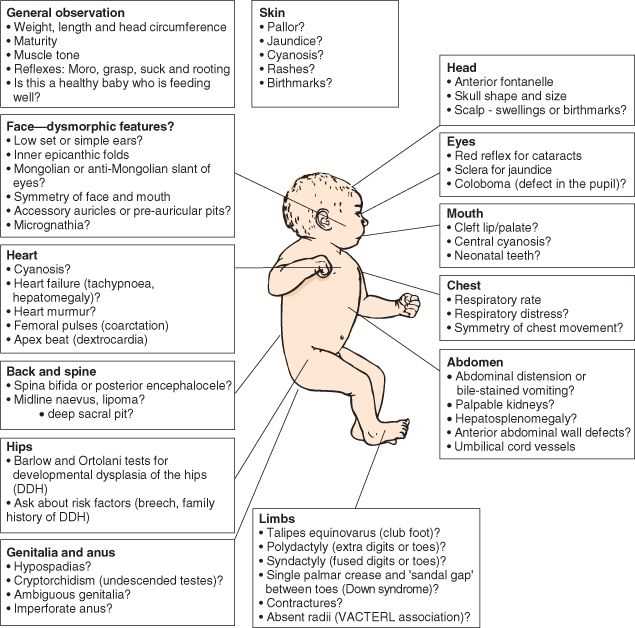
- Initial Observation: Begin by noting the infant’s overall appearance, including general demeanor and behavior. Any immediate physical signs such as color, posture, or movement should be recorded.
- Vital Signs: Record essential measurements like heart rate, respiratory rate, temperature, and weight. These parameters offer insights into the infant’s overall health and stability.
- Physical Measurements: Document physical characteristics such as head circumference, length, and weight percentiles. This helps assess the infant’s growth and development.
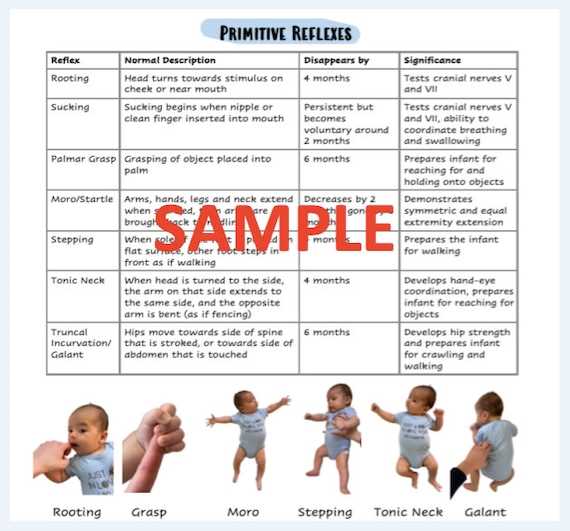
- Reflexes and Responses: Note key reflexes such as rooting, sucking, and grasping. Documenting these responses provides valuable information about the infant’s neurological development.
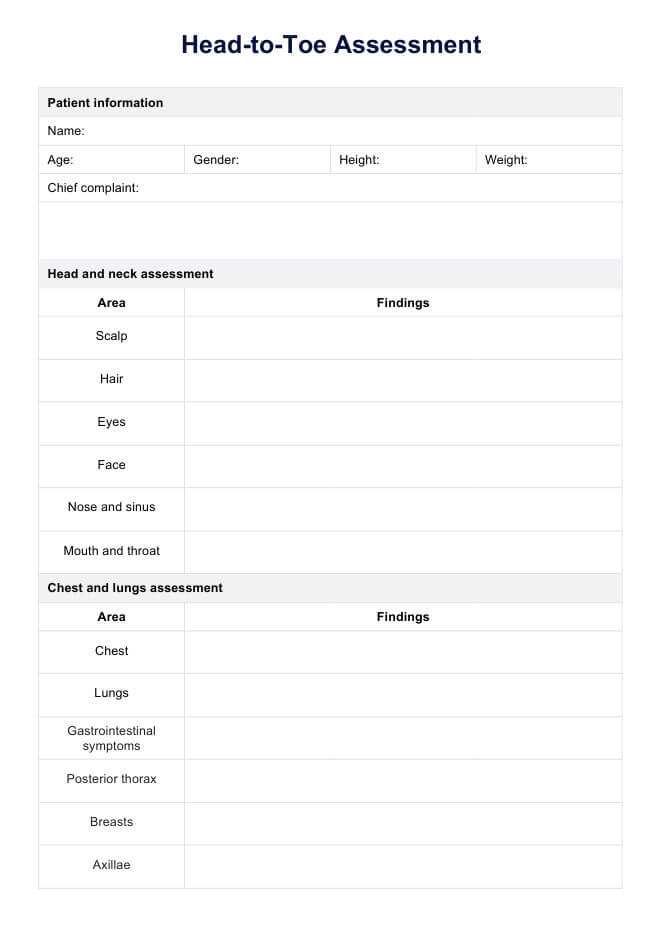
Common Findings to Include in the Report
- Skin Condition: Any rashes, birthmarks, or signs of infection should be thoroughly described, as these can be indicators of underlying health issues.
- Head and Neck: Document head shape, fontanelles, and any abnormalities such as swelling or signs of trauma. The neck should be evaluated for flexibility and symmetry.
- Chest and Abdomen: Record lung sounds, heart murmurs, and any abdominal abnormalities. Ensure the abdomen is soft and without distension.
- Extremities: Assess for any signs of abnormal limb development or deformities. This can include range of motion and muscle tone.
Each section should be clear and concise, with sufficient detail to allow for follow-up or comparison in future assessments. By following these guidelines, practitioners ensure that the health record serves as an accurate and reliable reference for ongoing care.
Understanding the Importance of Documentation
Accurate and thorough documentation is a fundamental aspect of any healthcare process. It ensures that all relevant information regarding an infant’s health is recorded and available for review. A well-documented assessment not only helps track the infant’s progress over time but also aids in identifying potential health issues that may require immediate attention or follow-up care.
Ensuring Consistency in Care
Comprehensive records provide a consistent baseline for healthcare providers, enabling them to make informed decisions based on past evaluations. Clear and reliable documentation ensures that multiple healthcare professionals, including specialists, are on the same page when it comes to treatment plans and interventions. This reduces the risk of errors and improves the continuity of care.
Legal and Professional Accountability
Proper documentation also serves a legal and professional function. It protects both the healthcare provider and the patient by providing an accurate record of assessments, interventions, and any actions taken. In case of any disputes or concerns, well-maintained records can serve as vital evidence that supports the medical decisions made during the evaluation.
By adhering to best practices in documentation, healthcare professionals can ensure that they provide the highest standard of care, while also safeguarding themselves and their patients through clear, precise, and accountable records.
Key Components of a Newborn Health Assessment
When assessing the health of an infant, several critical elements must be considered to ensure a comprehensive evaluation. These components provide essential insights into the baby’s overall health and development, helping healthcare professionals identify any immediate concerns or areas requiring further monitoring. A structured approach to documenting these elements ensures that all aspects are carefully reviewed and accurately recorded.
Essential Observations to Document
- General Appearance: Document the baby’s alertness, activity level, and responsiveness. These observations provide initial clues about the infant’s neurological and general health.
- Vital Signs: Include measurements such as heart rate, respiratory rate, temperature, and weight. These are fundamental for assessing the infant’s overall stability and well-being.
- Growth Parameters: Record the baby’s length, head circumference, and weight percentiles. These are important indicators of developmental progress.
Detailed Physical Evaluation
- Skin and Extremities: Inspect for any rashes, birthmarks, or signs of abnormal skin conditions. Also, check the limbs for symmetry, muscle tone, and movement.
- Head and Neck: Assess the size, shape, and fontanelles of the head. Ensure the neck shows no signs of stiffness or abnormalities in mobility.
- Chest and Abdomen: Listen for heart and lung sounds, and check the abdomen for any distension or tenderness.
By thoroughly documenting these key components, healthcare providers can develop a clear and accurate picture of the infant’s health status. This information is invaluable for ongoing care and for detecting any potential issues that may need attention in the future.
Preparing for a Newborn Health Assessment
Proper preparation is essential to ensure a smooth and thorough evaluation of an infant’s health. By organizing both the environment and the necessary tools ahead of time, healthcare providers can make the process more efficient and comfortable for the baby. Preparation also helps in gathering the required information to make accurate assessments and decisions during the evaluation.
Before conducting the assessment, it is important to have all necessary equipment ready, such as a scale, thermometer, stethoscope, and measuring tape. Ensuring the room is quiet, warm, and well-lit also helps to keep the baby calm and cooperative during the process. Having a well-planned approach allows the healthcare provider to focus on the task at hand, minimizing distractions and ensuring no critical aspects are overlooked.
Additionally, informing the parents or guardians about what to expect during the assessment can help alleviate any concerns and make the experience more comfortable for them. This collaborative approach ensures that both the healthcare provider and family are aligned in their expectations, leading to a more successful and less stressful evaluation.
Steps for Comprehensive Infant Evaluation
To conduct a thorough assessment of an infant’s health, it is essential to follow a structured and systematic approach. This process helps ensure that all critical aspects of the baby’s health are carefully evaluated and accurately documented. Each step contributes valuable information, from observing general well-being to checking for any physical abnormalities or developmental concerns.
Initial Observations and General Assessment
- Appearance: Observe the baby’s overall condition, including alertness, tone, and response to stimuli. These observations provide insight into the infant’s neurological function and general health.
- Vital Signs: Measure and record heart rate, respiratory rate, temperature, and weight. These basic readings are key indicators of the infant’s immediate health status.
- Behavior: Note the baby’s level of activity and responsiveness to touch or sound. This can reveal important information about sensory and motor development.
Detailed Physical Examination
- Skin Inspection: Check for any rashes, birthmarks, or signs of infection. The condition of the skin can reflect overall health and alert you to potential issues.
- Musculoskeletal System: Assess muscle tone, joint flexibility, and limb movement. This is crucial for identifying any potential birth defects or abnormal development.
- Head and Neck: Examine the head for symmetry, fontanelle condition, and any signs of trauma. Inspect the neck for any abnormalities in mobility or muscle tension.
- Chest and Abdomen: Listen to heart and lung sounds and check the abdomen for distension or tenderness. These signs are important for identifying respiratory or gastrointestinal issues.
By following these steps, healthcare providers ensure that each infant is assessed comprehensively. Thorough evaluations allow for early detection of any potential concerns, helping to provide the best possible care from the outset.
Common Findings in Infant Health Assessments
During an infant’s health evaluation, various common findings may be observed, ranging from normal developmental traits to potential concerns that require further monitoring. Recognizing these typical signs is essential for identifying the baby’s overall health status. It is important to document these findings accurately to distinguish between what is typical and what might signal a need for additional medical attention.
| Finding | Explanation | Action Required |
|---|---|---|
| Lanugo | Fine hair covering the body, often seen in premature infants or at birth. | Usually resolves on its own, no action required. |
| Fontanelle Softness | The soft spots on the head that allow for brain growth. | Normal; should be monitored for any abnormal bulging or sunken appearance. |
| Physiologic Jaundice | Yellowing of the skin or eyes, common in the first few days of life. | Typically resolves without treatment, but should be monitored for worsening symptoms. |
| Umbilical Cord Stump | The remnant of the umbilical cord that falls off in the first few weeks. | No intervention needed unless signs of infection are present, such as redness or discharge. |
| Grasp Reflex | Infants will automatically grasp an object placed in their hands. | Normal reflex, no action required. |
| Heart Murmur | A faint sound caused by blood flow, often heard in early assessments. | Usually benign; further evaluation may be necessary to rule out congenital heart defects. |
These findings are common and typically do not indicate serious health concerns. However, healthcare providers should remain vigilant, documenting and monitoring any changes or abnormalities. Early detection and careful observation are key to ensuring the best outcomes for infants.
Documenting Vital Signs in Infants
Accurate documentation of an infant’s vital signs is crucial for assessing their overall health and detecting any immediate concerns. These measurements provide valuable insight into the baby’s physiological state, helping healthcare providers monitor trends and identify potential issues that may require intervention. Properly recording these figures ensures that healthcare professionals have the necessary data to make informed decisions regarding care and treatment.
Key Vital Signs to Document
- Heart Rate: Measure the number of beats per minute. A normal range is typically 120-160 bpm, though this can vary depending on the infant’s activity level.
- Respiratory Rate: Count the number of breaths per minute. A typical range for a healthy infant is between 30 and 60 breaths per minute.
- Temperature: Monitor the infant’s body temperature, usually taken via axillary or rectal methods. The normal range is between 97.8°F (36.5°C) and 99.5°F (37.5°C).
- Weight: Regularly record the infant’s weight, as it is a key indicator of growth and development. Weight should be measured on the same scale each time for accuracy.
Proper Documentation Practices
- Use Consistent Units: Ensure all measurements are recorded in the appropriate units, such as bpm for heart rate and breaths per minute for respiratory rate.
- Record Time and Date: Always note the exact time and date of each measurement to track changes over time.
- Compare to Normal Ranges: When documenting, compare the readings to established normal ranges for infants. This helps to quickly identify any deviations that may require follow-up.
By thoroughly documenting these vital signs, healthcare providers can better monitor the infant’s health and ensure any necessary interventions are promptly implemented. Regular and accurate tracking is essential for maintaining high standards of care and addressing concerns as they arise.
Assessing Infant Reflexes and Responses
Evaluating reflexes and responses in infants is a critical component of assessing neurological and developmental health. These reflexes serve as early indicators of how the central nervous system is functioning and provide insight into the infant’s overall health. By observing and testing various reflexes, healthcare providers can identify any potential concerns or abnormalities that may require further attention or intervention.
Infants are born with a series of automatic reflexes that help them survive and adapt to their environment. These reflexes, such as grasping or rooting, are involuntary movements that occur in response to specific stimuli. The presence and strength of these reflexes are important in determining if the infant’s nervous system is developing normally.
Common Reflexes to Assess
- Moro Reflex: Often referred to as the startle reflex, this occurs when the infant feels a sudden loss of support or hears a loud noise. The baby will extend their arms, then quickly bring them back in.
- Rooting Reflex: This reflex occurs when the infant’s cheek is stroked, prompting them to turn their head and open their mouth as if seeking the breast for feeding.
- Grasp Reflex: When an object is placed in the infant’s palm, they will instinctively grasp it tightly, showing strength and coordination in their hands.
- Babinski Reflex: When the sole of the foot is stroked, the infant will spread their toes, which is a normal response during the first few months.
Assessing these reflexes provides valuable information about the infant’s motor and sensory development. Most reflexes will gradually disappear as the baby’s brain and nervous system mature, which is a normal part of development. However, the persistence of certain reflexes beyond the expected timeframe could be a sign of neurological concerns, requiring further evaluation.
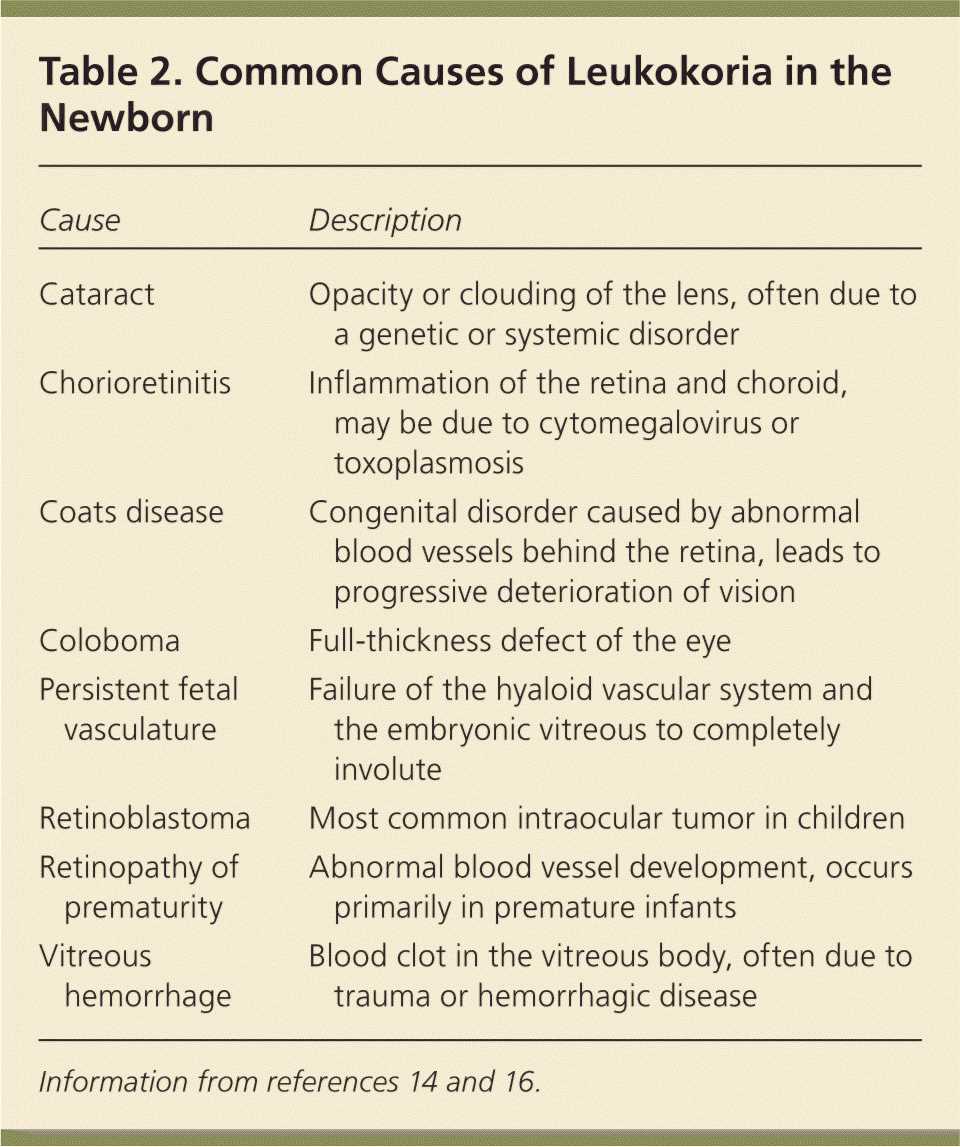
Identifying Abnormalities in Infant Health
Recognizing irregularities in an infant’s health is crucial for early intervention and proper care. Some signs of concern may be subtle, while others may be more obvious, but each can significantly impact the baby’s development if not addressed. Thorough observation and understanding of normal growth patterns are key to identifying any potential issues, which allows for timely medical intervention when necessary.
Abnormal findings can arise in various areas of health, including vital signs, physical development, and reflex responses. Identifying these issues requires not only a keen understanding of typical infant health patterns but also the ability to recognize when a deviation from the norm may indicate a need for further investigation or treatment.
Common Abnormalities to Look For
- Persistent Jaundice: If yellowing of the skin or eyes lasts longer than usual, it could indicate liver or blood problems that require further testing.
- Irregular Heart Rate: A heart rate that is significantly higher or lower than the normal range may suggest cardiovascular issues, necessitating additional monitoring.
- Abnormal Respiratory Patterns: Rapid breathing, labored breathing, or pauses in breathing might indicate respiratory distress or other underlying conditions.
- Excessive Weight Loss: A significant drop in weight within the first few days could be a sign of feeding difficulties or other metabolic concerns.
- Abnormal Reflex Responses: If reflexes such as the Moro or rooting reflexes are absent or delayed, it could signal neurological concerns that require attention.
When abnormalities are detected, prompt action is crucial. This may involve further examination, diagnostic testing, or referrals to specialists. Early identification of any irregularities ensures that the infant receives the appropriate care, enhancing the chances of positive health outcomes.
Best Practices for Writing a Clear Report
Creating a clear and concise report is essential for conveying important health information accurately. A well-written document not only provides a detailed account of the assessment but also ensures that the information is easily understood by other healthcare professionals involved in the care process. By following best practices, one can ensure the report is both thorough and accessible, reducing the risk of misinterpretation and enhancing patient care.
Key Tips for Clarity and Precision
- Use Simple and Direct Language: Avoid complex medical jargon unless necessary. Clear and straightforward language improves comprehension, especially for readers who may not be familiar with specialized terms.
- Organize Information Logically: Structure the report in a systematic way, beginning with the most relevant findings, followed by less critical details. This helps readers easily locate key information.
- Be Concise: While detail is important, avoid unnecessary repetition. Focus on including the most relevant observations and measurements.
- Include Objective Measurements: Document all vital signs, reflexes, and physical findings in precise numerical terms or clear descriptions. This provides an objective basis for future evaluations.
- Highlight Abnormalities: Clearly distinguish any findings that deviate from normal patterns. Use bold or underlined text to make these stand out, ensuring they are easily noticed.
- Review and Proofread: Always review your report for accuracy and clarity before submission. Proofreading ensures that any errors are caught and corrected, preventing confusion or misinformation.
Example of a Well-Structured Report
| Category | Finding | Remarks |
|---|---|---|
| Heart Rate | 140 bpm | Normal range |
| Respiratory Rate | 45 breaths/min | Normal range |
| Temperature | 98.2°F | Normal range |
| Grasp Reflex | Present | Normal |
| Abnormal Findings | Persistent jaundice | Further monitoring required |
By adhering to these best practices, you can ensure that the report is clear, professional, and effective in conveying critical health information, contributing to the overall care and management of the patient.
Tips for Accurate Infant Health Documentation
Accurate documentation is essential for ensuring that every aspect of a baby’s health is properly recorded and communicated. A precise and thorough report not only aids in effective decision-making but also serves as a valuable reference for future assessments. By following some simple but effective guidelines, healthcare professionals can minimize the risk of errors and enhance the quality of care provided.
Key Strategies for Accurate Documentation
- Ensure Consistent Measurements: Always use standardized tools and techniques to measure vital signs and physical characteristics. Consistent methods help avoid discrepancies and ensure data reliability.
- Record Observations Promptly: Write down your findings as soon as possible after each assessment. Delaying documentation increases the chance of forgetting key details or misinterpreting information.
- Be Specific and Detailed: When documenting findings, include all relevant details such as exact measurements, timing, and the condition of the baby. General statements can lead to confusion or missed concerns.
- Avoid Ambiguity: Use clear and unambiguous language. Phrases such as “normal” or “within range” should be paired with specific values or observations to provide clarity.
- Use Objective Terms: Stick to objective descriptions of what was observed. Avoid subjective language or personal opinions, as this can lead to misunderstandings or inaccuracies in medical decision-making.
- Double-Check for Accuracy: After completing the documentation, take a moment to review the report. Ensure that all values and descriptions match your observations and that no important detail is overlooked.
By focusing on accuracy and clarity, healthcare professionals can ensure that the documentation serves as an effective tool for managing infant health. This practice not only enhances patient care but also ensures a more seamless transition between different caregivers and medical professionals.
How to Record Physical Growth Data
Accurately documenting an infant’s growth is essential for monitoring overall health and development. This process involves tracking key measurements that reflect the child’s physical progress, ensuring that any deviations from expected patterns are identified early. Proper recording of growth data provides a clear picture of the infant’s well-being and assists healthcare providers in making informed decisions regarding care and interventions.
Key Growth Indicators to Record
- Weight: Measure the infant’s weight using a calibrated scale. Record the exact weight to the nearest gram or ounce, depending on your measurement system. This is one of the most important indicators of health and development.
- Length: Use a standardized measuring board or infantometer to measure the infant’s length. Ensure that the baby is positioned properly, with the head and feet aligned to avoid measurement errors.
- Head Circumference: Measure the circumference of the head with a soft, flexible tape. Record this measurement to track brain development and detect any abnormalities.
Best Practices for Accurate Recording
- Ensure Consistency: Use the same tools and methods for each measurement to reduce variability and ensure the accuracy of the data.
- Record Immediately: Write down measurements right after performing the assessment to avoid errors or forgetfulness.
- Include Units: Always specify the units used for measurement (e.g., centimeters, kilograms, ounces) to prevent confusion.
- Monitor Trends: When documenting, compare the current measurements with previous ones to detect any trends or signs of abnormal growth patterns.
By carefully recording these key indicators and following standardized methods, healthcare providers can ensure they are capturing accurate growth data. This is essential for monitoring the infant’s development and ensuring they are on track with their milestones.
Understanding the Role of Family History
Family history plays a crucial role in assessing the overall health and well-being of an infant. By understanding the medical background of immediate family members, healthcare providers can identify potential genetic conditions, hereditary diseases, or environmental factors that may influence the child’s development. This information helps create a more comprehensive care plan, allowing for early detection and timely intervention when necessary.
Gathering a thorough family health history involves more than just asking about common conditions; it includes looking for patterns of illness that may suggest a hereditary predisposition. Knowing whether relatives have experienced conditions such as cardiovascular issues, metabolic disorders, or autoimmune diseases can provide valuable insights into the infant’s health risks.
Why Family History Matters
- Identifying Genetic Risks: Certain conditions are passed down through families, and knowing this can help anticipate potential health challenges.
- Early Detection: Family history can serve as a warning sign for diseases that might not be visible immediately, allowing for preventive measures or early screening.
- Informed Decision-Making: Understanding hereditary health issues enables healthcare providers to offer advice on managing potential risks and tailoring treatments.
How to Collect Family History Effectively
- Ask Specific Questions: Inquire about particular conditions, such as cancer, diabetes, or neurological disorders, and whether they have occurred in close relatives.
- Document Health Patterns: Keep detailed records of the family health background, noting any recurring illnesses or disorders that may indicate genetic tendencies.
- Include Both Sides of the Family: Gather information about both maternal and paternal relatives to get a complete picture of inherited health factors.
Integrating family history into the assessment process ensures that healthcare professionals are equipped with the knowledge to provide optimal care and anticipate potential health concerns, making it a vital aspect of overall healthcare management for infants.
Organizing Findings for Clinical Review
Effectively organizing and presenting clinical findings is essential for ensuring that healthcare providers can quickly assess an infant’s health status. A well-structured report enables clinicians to identify key issues, track developmental progress, and make informed decisions. Organizing the data clearly and logically also facilitates communication among the healthcare team, ensuring that critical information is not overlooked.
To ensure clarity and comprehensiveness, it’s important to categorize the findings based on their significance and relevance to the patient’s overall health. This approach not only helps healthcare professionals quickly identify areas requiring attention but also supports the identification of trends over time.
Categories for Organizing Findings
| Category | Description |
|---|---|
| Growth and Development | Record measurements such as weight, length, and head circumference. Note if growth patterns align with typical milestones. |
| Vital Signs | Include heart rate, respiratory rate, temperature, and blood pressure, providing a snapshot of the infant’s immediate health status. |
| Reflexes and Responses | Document reflex tests such as rooting, sucking, and grasping to assess neurological function and motor responses. |
| Physical Appearance | Note any visible physical abnormalities or features that may require further examination, such as skin conditions or facial symmetry. |
| Family History | Include relevant family medical history that could influence the infant’s health or suggest genetic predispositions to certain conditions. |
Best Practices for Documentation
- Use Clear and Concise Language: Avoid medical jargon and provide straightforward descriptions of the findings.
- Group Related Information: Cluster similar data together to streamline the review process, making it easier to identify patterns or concerns.
- Highlight Abnormal Findings: Ensure that any unusual or concerning findings are clearly marked and prioritized for further assessment.
By organizing clinical findings in a structured manner, healthcare professionals can ensure that all relevant information is easily accessible, leading to better-informed clinical decisions and more effective care management.
Challenges in Newborn Physical Assessments
Conducting a thorough evaluation of an infant’s health can present numerous challenges. The process requires careful attention to detail, as well as the ability to distinguish between typical development and potential health concerns. The delicate nature of the assessment, combined with the varying presentation of conditions in young infants, makes this task both complex and critical for ensuring optimal care.
Several factors contribute to the challenges faced during these evaluations. These can include the infant’s inability to communicate symptoms directly, the subtle presentation of certain conditions, and the pressure to identify both immediate and long-term health concerns. Additionally, healthcare providers must navigate the varied physical and emotional responses of both the infant and the parents, which can complicate the process.
Key Challenges in Assessment
- Limited Communication: Infants cannot verbalize their discomfort or symptoms, making it harder for clinicians to identify underlying health issues.
- Subtle Indicators: Some medical conditions may not be immediately apparent and require careful observation over time.
- Environmental Factors: A clinical setting can be stressful for both the infant and the parents, which may affect the accuracy of the findings.
- Developmental Variations: Infants grow and develop at different rates, so variations in their physical condition might not necessarily be cause for concern.
Approaches to Overcome Challenges
- Thorough Observation: Careful monitoring and repeated assessments help detect subtle changes or abnormalities over time.
- Parental Input: Engaging with parents to understand any concerns they may have can provide valuable insights into the infant’s health.
- Collaboration: Consulting with pediatric specialists can help resolve complex cases or conditions that are not easily diagnosed during initial assessments.
By recognizing and addressing these challenges, healthcare providers can improve the accuracy and reliability of infant health assessments, ultimately contributing to better outcomes for the child.
Reviewing a Newborn Exam Write-Up
When evaluating a report documenting a recent health evaluation of an infant, it’s crucial to ensure that all aspects of the assessment are accurately and clearly presented. A comprehensive review helps to identify any areas of concern or discrepancies that may need further attention. The goal is to ensure the information is thorough, precise, and reflects the overall well-being of the infant, along with any potential issues that may require follow-up.
Key areas to focus on during the review include the completeness of the data, clarity in describing the observed findings, and the coherence of the narrative that ties together different aspects of the assessment. Ensuring that all relevant information is included, such as vital signs, developmental milestones, and physical appearance, is vital to forming a full picture of the infant’s health. Additionally, clear documentation of any concerns or abnormal findings should be present to facilitate appropriate follow-up care.
During the review process, it is also important to assess how well the report communicates the clinical reasoning behind the conclusions drawn. This involves verifying whether any potential issues have been flagged for further observation or action and ensuring that the tone remains professional and objective throughout. A well-documented evaluation provides the necessary foundation for making informed decisions about the care and treatment of the infant.
Using Technology for Efficient Documentation
In today’s healthcare environment, technology plays a crucial role in enhancing the efficiency and accuracy of recording medical assessments. Digital tools allow healthcare professionals to streamline the process of documenting patient evaluations, ensuring that essential information is captured quickly and accurately. These technological advancements also help reduce human error and improve the accessibility of patient records, making it easier to retrieve and share information as needed.
Electronic health records (EHRs) are one of the most commonly used technologies for efficient documentation. EHR systems not only store patient information securely but also provide templates and checklists that guide healthcare providers through the necessary steps of recording an assessment. This ensures that no key details are overlooked while also saving time by automating routine tasks. Additionally, these systems can generate reports instantly, making the documentation process faster and more reliable.
Another useful tool is voice recognition software, which allows healthcare professionals to dictate their observations directly into the system. This can significantly speed up the documentation process, especially in busy clinical settings. By reducing the need for manual entry, voice recognition helps to ensure that the focus remains on patient care while still maintaining comprehensive and accurate records.