Cardiovascular Physiology Exam Questions and Answers
The study of how the heart and blood vessels work together to maintain circulation is essential for anyone pursuing a deeper understanding of human health. This area of knowledge delves into the complex mechanisms that regulate blood flow, pressure, and oxygen delivery to various tissues. A strong grasp of these concepts is crucial for anyone preparing for assessments in related fields.
By mastering the core principles behind heart function, you can better comprehend how the body adapts to different conditions, including exercise and stress. The interactions between various organs and systems form a delicate balance that ensures proper nutrient and gas exchange. With the right insights, it becomes easier to analyze various scenarios and improve diagnostic skills.
To excel in this subject, it is important to review common topics, recognize patterns, and understand how different factors influence overall function. The following sections will guide you through essential themes, highlighting key points to help solidify your knowledge and enhance performance in evaluations.
Cardiovascular Physiology Exam Questions and Answers
For anyone preparing for assessments in heart function and circulation, it is essential to familiarize oneself with the key concepts that are often tested. A solid understanding of how the body regulates blood flow, pressure, and oxygen distribution is crucial for success in this area. Practicing common topics will not only enhance comprehension but also help anticipate the types of challenges one may face during evaluations.
In this section, we will explore various scenarios and situations that are frequently examined. By examining the underlying principles of blood circulation, heart rate regulation, and vascular dynamics, you can sharpen your analytical skills and apply theoretical knowledge to practical situations. Whether it’s understanding how heartbeats are controlled or how different factors impact blood pressure, being prepared for these topics is essential for demonstrating mastery.
Each section focuses on a different aspect of heart function, offering explanations, followed by relevant exercises. Emphasis will be placed on critical thinking and application, with a focus on practical approaches to answering typical evaluation tasks. By reviewing these areas, you will build a strong foundation for tackling similar challenges with confidence.
Understanding Heart Function and Circulation
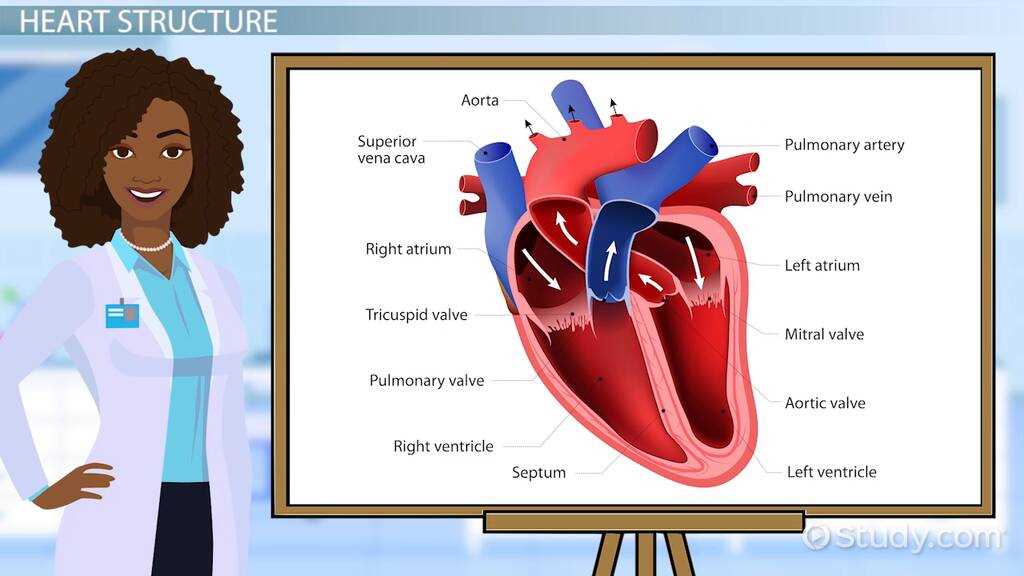
The heart plays a central role in maintaining the flow of blood throughout the body. This system of pumping blood is vital for delivering oxygen and nutrients to tissues and removing waste products. Understanding how the heart works, along with the mechanisms that govern blood movement, is essential for assessing overall health and diagnosing potential issues.
Mechanisms of Blood Flow Regulation
Blood circulation is regulated by a complex interplay of various factors, including pressure gradients, vessel elasticity, and the rhythm of the heart. The heart’s pumping action creates pressure that drives blood through arteries and veins, ensuring that oxygen-rich blood reaches the organs and tissues that need it most. Additionally, feedback mechanisms such as baroreceptor reflexes help maintain a steady blood pressure, adapting to changes in posture or activity levels.
The Role of the Heart’s Electrical System
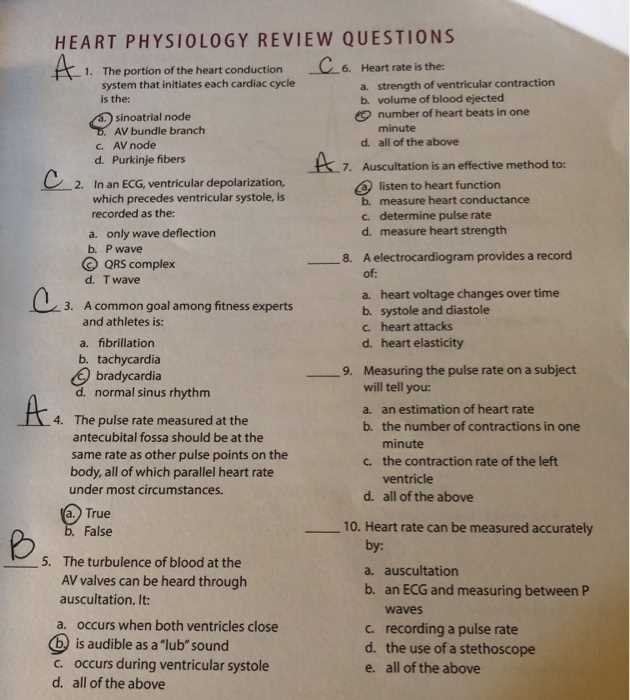
The electrical impulses that trigger each heartbeat are integral to the heart’s function. These impulses begin in the sinoatrial node and propagate through the heart muscle, ensuring coordinated contractions. Any disruption to this electrical system can lead to irregular heartbeats, or arrhythmias, which can affect blood circulation and overall health. Understanding the electrical control of the heart is critical for recognizing and addressing such conditions.
Key Concepts in Blood Pressure Regulation
The regulation of blood pressure is a critical aspect of maintaining homeostasis within the body. Proper control ensures that organs receive adequate blood flow while preventing damage to the vascular system. Several mechanisms, including neural, hormonal, and vascular factors, work together to maintain an optimal pressure level, adapting to changing physical demands or conditions.
Neural Control and Feedback Mechanisms
The nervous system plays an essential role in monitoring and adjusting blood pressure. The baroreceptors located in the carotid sinus and aortic arch detect changes in pressure and send signals to the brain. The brain then activates the autonomic nervous system to make adjustments, either constricting or dilating blood vessels and influencing heart rate to stabilize pressure.
Hormonal Influence on Blood Pressure
Hormones, such as adrenaline, aldosterone, and antidiuretic hormone (ADH), significantly influence blood pressure regulation. These substances can alter the diameter of blood vessels or adjust the volume of fluids in the body, helping to maintain steady pressure levels during periods of stress or dehydration.
| Hormone | Effect on Blood Pressure |
|---|---|
| Adrenaline | Increases heart rate and vasoconstriction, raising blood pressure |
| Aldosterone | Promotes sodium retention, increasing blood volume and pressure |
| ADH | Increases water retention by kidneys, raising blood volume and pressure |
The Role of Blood Vessels in Circulation
Blood vessels are integral components of the circulatory system, serving as the pathways through which blood flows to various tissues and organs. These structures are crucial for maintaining effective transport of oxygen, nutrients, and waste products. The function of blood vessels goes beyond simple conduit; they are involved in regulating blood pressure, directing blood flow, and facilitating exchanges at the cellular level.
Types of Blood Vessels
There are three primary types of blood vessels, each with a specific role in circulation:
- Arteries: Carry oxygen-rich blood from the heart to the body. They are equipped with thick, muscular walls to withstand the pressure generated by the heart’s contractions.
- Veins: Transport deoxygenated blood back to the heart. These vessels have thinner walls and rely on muscle contractions to help return blood against gravity.
- Capillaries: The smallest vessels, connecting arteries and veins. They facilitate nutrient and gas exchange between blood and tissues.
Vascular Health and Its Impact
Maintaining the health of blood vessels is essential for overall well-being. Factors like cholesterol levels, blood pressure, and inflammation can affect vessel function. For instance, high blood pressure can damage arterial walls, leading to a condition called atherosclerosis. Conversely, healthy blood vessels support smooth blood flow, ensuring proper oxygen and nutrient delivery to tissues.
- Atherosclerosis: A condition in which fatty deposits build up on the arterial walls, narrowing the vessels and restricting blood flow.
- Hypertension: Chronic high blood pressure that puts strain on the heart and arteries, increasing the risk of stroke and heart disease.
- Endothelial Dysfunction: Damage to the inner lining of blood vessels, which can lead to problems with blood flow and clotting.
Examining Cardiac Output and Stroke Volume
The heart’s ability to pump blood effectively is a key factor in maintaining adequate circulation throughout the body. Two important metrics in assessing heart function are the volume of blood pumped per minute and the amount of blood ejected with each heartbeat. These parameters play a crucial role in determining overall cardiovascular health and efficiency.
Cardiac Output: The Total Volume Pumped
Cardiac output refers to the total volume of blood that the heart pumps in one minute. It is a critical indicator of how well the heart is meeting the body’s demands for oxygen and nutrients. Cardiac output is influenced by factors such as heart rate and stroke volume. An increase in either of these can elevate cardiac output, ensuring that more blood reaches tissues, especially during physical exertion.
Stroke Volume: The Blood Ejected Per Beat

Stroke volume is the amount of blood ejected from the heart with each contraction. It is determined by several factors, including preload (the initial stretch of the heart muscle), afterload (the resistance the heart must overcome to eject blood), and contractility (the strength of the heart’s contraction). A healthy stroke volume ensures that the heart is efficiently delivering oxygenated blood to the body’s tissues, while any imbalance can affect overall circulation.
Changes in stroke volume can indicate underlying health issues. For example, a decreased stroke volume may result from heart conditions such as heart failure, where the heart is unable to contract effectively. Conversely, an elevated stroke volume may occur in well-conditioned athletes, as their hearts are more efficient at pumping blood.
Understanding the Cardiac Cycle
The heart operates through a repetitive sequence of events that allow it to pump blood efficiently to all parts of the body. This cycle involves a series of contractions and relaxations that are precisely timed to ensure blood flows smoothly through the heart’s chambers and into the circulatory system. A thorough understanding of this process is essential for grasping how the heart supports overall health and function.
The cycle begins with the relaxation phase, where the heart chambers fill with blood. Following this, the heart contracts, pushing the blood into the arteries. These alternating phases of relaxation and contraction are critical for maintaining continuous blood flow. The process is driven by electrical impulses that ensure the heart beats rhythmically and synchronously, allowing optimal blood circulation.
Disruptions in the cardiac cycle, such as arrhythmias or abnormal contractions, can impair the heart’s ability to pump blood effectively. Understanding each phase helps in diagnosing and managing various heart conditions, from mild irregularities to more severe heart diseases.
Questions on Heart Rate Variability
Heart rate variability (HRV) refers to the fluctuations in the time intervals between heartbeats. It is a valuable indicator of the body’s ability to adapt to changes in the environment and internal states. HRV is influenced by factors such as stress, physical activity, and overall health. Analyzing these variations can provide insights into autonomic nervous system function and cardiovascular health.
Why Is HRV Important?
HRV is often considered a measure of heart health and the body’s resilience to stress. Higher variability typically indicates better cardiovascular fitness and a more adaptable autonomic nervous system. In contrast, low HRV can be associated with stress, fatigue, and even chronic health conditions such as heart disease.
Factors That Affect HRV
Several factors can influence HRV, including:
- Physical Activity: Regular exercise tends to increase HRV, reflecting better heart function and autonomic balance.
- Stress Levels: Chronic stress can lower HRV, signaling an overactive sympathetic nervous system.
- Sleep Quality: Poor sleep can negatively impact HRV, as recovery during sleep supports autonomic function.
Monitoring HRV can offer valuable insights into the state of your heart and autonomic regulation, making it an important factor in assessing overall wellness.
The Physiology of Blood Flow Distribution
The body carefully regulates the flow of blood to different tissues, ensuring that each organ receives the appropriate amount of oxygen and nutrients based on its needs. This dynamic process involves the constriction and dilation of blood vessels, which directs blood to where it is most required at any given moment. Understanding how blood is distributed throughout the body is crucial for comprehending how the circulatory system responds to varying demands, such as during exercise or rest.
Blood flow distribution is influenced by several factors, including metabolic demand, neural control, and local regulatory mechanisms. During physical activity, for example, more blood is directed to the muscles to support increased energy needs, while less blood flows to non-essential organs. Conversely, during periods of rest, the body shifts resources to maintain homeostasis and support recovery. The ability of the circulatory system to adjust blood flow efficiently ensures that each tissue functions optimally under various conditions.
Mechanisms of Vascular Resistance and Compliance
The ability of blood vessels to adjust their diameter and respond to changes in pressure is fundamental to maintaining efficient blood circulation. Two key factors that influence blood flow are vascular resistance and compliance. Vascular resistance refers to the opposition to blood flow within the vessels, while compliance describes the ability of blood vessels to expand and contract in response to changes in blood pressure. Together, these mechanisms help regulate the distribution of blood throughout the body and maintain proper pressure levels within the circulatory system.
Vascular Resistance: Key Factors
Resistance in the blood vessels is determined by several factors:
- Vessel Diameter: The smaller the vessel’s diameter, the greater the resistance to blood flow. This is why constriction of blood vessels can significantly increase vascular resistance.
- Blood Viscosity: Thicker blood, such as that with higher levels of red blood cells, increases resistance to flow.
- Vessel Length: Longer blood vessels provide more resistance to blood flow, although this factor is generally fixed in the body.
Vascular Compliance: Flexibility of Blood Vessels
Vessel compliance is the ability of blood vessels to stretch and accommodate the volume of blood being pumped through them. It is crucial for managing the changes in pressure that occur during the cardiac cycle. Key aspects that influence compliance include:
- Elasticity of Vessel Walls: Healthy, elastic arteries can expand and recoil to maintain stable blood pressure. Stiffness, often due to aging or disease, reduces compliance.
- Blood Volume: A higher volume of blood leads to increased vessel expansion, while lower blood volume reduces the stretch of the vessels.
Both vascular resistance and compliance work in tandem to ensure that the circulatory system adapts to the body’s varying needs, from rest to intense activity, and maintains optimal blood flow and pressure balance.
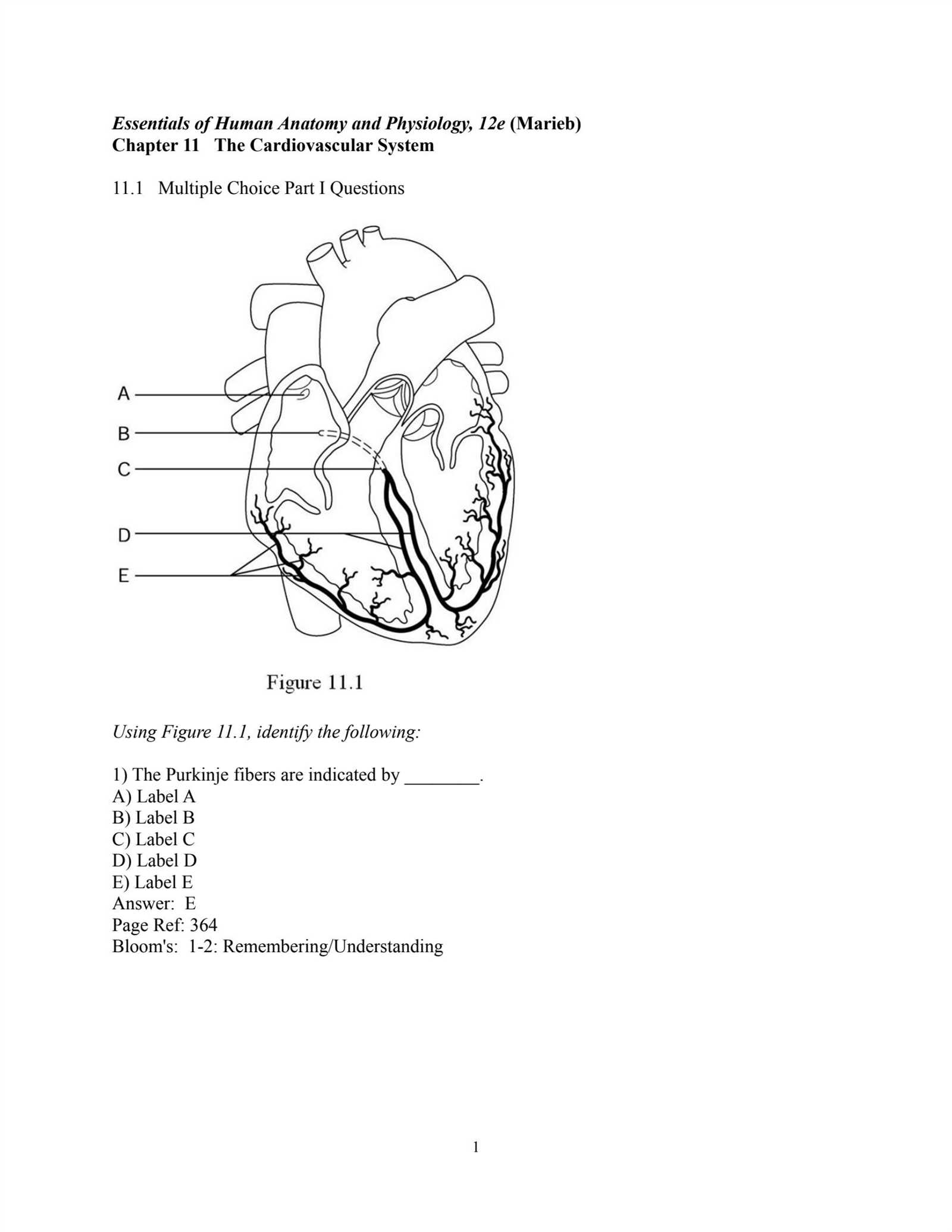
Cardiac Electrophysiology and ECG Interpretation
The electrical activity of the heart plays a vital role in coordinating its rhythmic contractions. Understanding the underlying mechanisms that generate and propagate these electrical signals is essential for diagnosing various heart conditions. The heart’s electrical impulses trigger each beat, ensuring that the atria and ventricles contract in a synchronized manner, allowing for effective blood circulation.
Electrocardiography (ECG) is a key diagnostic tool used to monitor and interpret the electrical activity of the heart. By placing electrodes on the skin, an ECG records the waves of electrical signals as they travel through the heart. These signals provide important information about heart rate, rhythm, and potential abnormalities such as arrhythmias or conduction disorders. Proper interpretation of ECG patterns helps healthcare providers detect irregularities, guiding treatment decisions for patients with cardiac concerns.
Heart Murmurs and Their Clinical Significance
Heart murmurs are abnormal sounds heard during a heartbeat, often detected by a stethoscope. These sounds result from turbulent blood flow within the heart or major blood vessels, which can occur for various reasons. While some murmurs are harmless, others can indicate underlying heart conditions. Understanding the cause of a murmur is crucial for determining its clinical significance and whether further medical evaluation or treatment is needed.
Murmurs are generally classified into two categories: innocent (or functional) murmurs, which do not suggest heart disease, and pathological murmurs, which may signal structural heart problems. The intensity, timing, and pitch of the sound provide valuable clues to healthcare providers, aiding in diagnosis and treatment planning.
Types of Heart Murmurs
Heart murmurs are commonly categorized based on their timing in the cardiac cycle and the underlying cause:
- Systolic Murmurs: These occur during the contraction phase of the heart and can be caused by issues such as valve stenosis or regurgitation.
- Diastolic Murmurs: These occur during the relaxation phase and may indicate conditions like valve insufficiency or narrowing.
- Continuous Murmurs: Heard throughout the cardiac cycle, these murmurs may be due to abnormal shunts or persistent ductus arteriosus.
Clinical Significance of Heart Murmurs
The clinical relevance of a heart murmur depends on its characteristics, including:
- Intensity: Louder murmurs may indicate a more significant issue, while softer murmurs could be benign.
- Pitch and Quality: A high-pitched murmur suggests a faster blood flow, often related to valve narrowing, while a low-pitched murmur may indicate regurgitation.
- Timing: Whether the murmur occurs during systole or diastole helps identify specific heart conditions.
Not all heart murmurs require intervention, but identifying the cause is essential for ensuring proper management and preventing potential complications. Healthcare providers often use diagnostic tools like echocardiography to evaluate the structural and functional aspects of the heart in greater detail.
Regulation of Respiratory and Circulatory Systems
The body maintains homeostasis through complex interactions between various systems. The regulation of both the respiratory and circulatory systems is essential to ensure that oxygen is efficiently delivered to tissues and carbon dioxide is removed. These systems work closely together, with the circulatory system transporting oxygen and nutrients while the respiratory system is responsible for the exchange of gases. Proper regulation is crucial for maintaining blood pressure, gas levels, and overall body function, especially under varying physiological conditions such as exercise or stress.
The mechanisms that control these systems involve feedback loops, sensors, and central control centers within the brain. These systems can adjust their activity in response to signals such as changes in oxygen or carbon dioxide concentrations, blood pH, and blood pressure. The integration of both systems allows for coordinated responses to meet the metabolic demands of the body.
Key Factors in Regulation
Several factors influence the regulation of both the respiratory and circulatory systems:
| Factor | Effect on Regulation |
|---|---|
| Oxygen Levels | Low oxygen levels stimulate both systems to increase respiration and blood flow to tissues. |
| Carbon Dioxide Levels | High CO2 levels lead to increased breathing rate and adjustments in blood vessel dilation to promote gas exchange. |
| Blood pH | Decreased pH (acidosis) triggers increased ventilation to expel CO2, helping to restore balance. |
| Blood Pressure | Baroreceptors monitor blood pressure, signaling adjustments in heart rate and blood vessel constriction or dilation. |
Integrated Control Systems
The brain plays a central role in coordinating the regulation of these systems. The medulla oblongata and pons in the brainstem are responsible for monitoring blood gases and sending signals to the respiratory muscles and the heart. These areas of the brain also regulate the autonomic nervous system, which controls involuntary functions such as heart rate and breathing patterns. The hypothalamus further integrates sensory input, coordinating the body’s responses to both environmental factors and internal conditions.
Overall, the regulation of the respiratory and circulatory systems ensures efficient delivery of oxygen and removal of waste products. Understanding these mechanisms is vital for diagnosing and managing conditions such as respiratory failure, hypertension, and circulatory disorders.
Factors Affecting Oxygen and Carbon Dioxide Transport
The effective transport of oxygen and carbon dioxide throughout the body is essential for maintaining cellular function and overall health. Several factors influence the efficiency with which these gases are carried by the blood, ensuring proper delivery to tissues and removal of waste products. These factors include the characteristics of the blood, the efficiency of the respiratory and circulatory systems, and the conditions of the tissues themselves.
The transport of gases is influenced by variables such as hemoglobin concentration, blood pH, temperature, and the partial pressures of oxygen and carbon dioxide. These elements interact with each other, impacting the ability of the blood to bind to oxygen and carbon dioxide, as well as the release of these gases at the tissue level. Understanding these factors is crucial for understanding how the body adapts to different environments, such as during physical activity or in response to disease.
Key Factors in Gas Transport
The following factors significantly impact the transport of oxygen and carbon dioxide:
| Factor | Impact on Gas Transport |
|---|---|
| Hemoglobin Concentration | A higher hemoglobin level increases the blood’s capacity to carry oxygen, while lower levels reduce oxygen delivery. |
| Partial Pressure of Oxygen (pO2) | Higher pO2 increases the affinity of hemoglobin for oxygen, enhancing oxygen uptake in the lungs. |
| Partial Pressure of Carbon Dioxide (pCO2) | Increased pCO2 promotes the release of oxygen from hemoglobin to tissues and enhances the uptake of carbon dioxide for exhalation. |
| Blood pH | Acidic conditions (lower pH) reduce hemoglobin’s affinity for oxygen, aiding oxygen release in tissues but also affecting overall gas transport efficiency. |
| Temperature | Higher temperatures decrease oxygen affinity in hemoglobin, facilitating oxygen release to active tissues, such as muscles during exercise. |
Impact of Environmental and Health Factors
Environmental conditions, such as altitude, and health conditions like anemia or respiratory diseases, can further influence the efficiency of gas transport. At higher altitudes, for example, the lower atmospheric oxygen levels require adjustments in the body’s ability to absorb and distribute oxygen. Similarly, conditions like chronic obstructive pulmonary disease (COPD) or heart failure can impair the transport of oxygen and carbon dioxide, leading to difficulty in meeting the metabolic demands of the body.
These interactions highlight the importance of maintaining optimal conditions for oxygen and carbon dioxide transport to support cellular activities and overall health. Understanding these factors provides insight into how the body compensates for challenges and adapts to changing conditions.
Exploring the Role of the Lymphatic System
The lymphatic system plays a crucial role in maintaining fluid balance, supporting the immune system, and facilitating the removal of waste products from the body. This network of vessels, tissues, and organs is essential for defending the body against infections and other harmful agents. It works in tandem with the circulatory system to transport lymph, a clear fluid that contains immune cells, proteins, and waste materials.
One of the primary functions of the lymphatic system is to collect excess interstitial fluid from tissues and return it to the bloodstream. By doing so, it helps maintain proper blood volume and pressure. Additionally, the system is involved in filtering lymph to remove pathogens and other harmful substances before they can enter the bloodstream. Lymph nodes, which are spread throughout the body, act as filters and play an active role in immune responses.
Key Components of the Lymphatic System
- Lymph: A fluid containing white blood cells, waste, and other substances, which circulates through the lymphatic vessels.
- Lymphatic Vessels: A network of vessels that transport lymph throughout the body, similar to how veins carry blood.
- Lymph Nodes: Small, bean-shaped structures that filter lymph and house immune cells to help fight infections.
- Spleen: An organ that filters blood, removes old red blood cells, and stores immune cells to aid in fighting infections.
- Thymus: An organ where certain white blood cells, called T-cells, mature and become functional in immune responses.
Immune System Support
In addition to its role in fluid balance, the lymphatic system is integral to the body’s defense mechanisms. It transports immune cells such as lymphocytes, which are crucial for identifying and attacking pathogens. The lymph nodes, spleen, and tonsils work in coordination to filter and destroy harmful microorganisms. When an infection occurs, the lymphatic system activates an immune response, increasing the production of white blood cells and antibodies to combat the threat.
Fluid Homeostasis
The lymphatic system also plays a vital role in maintaining the body’s fluid homeostasis. By draining excess fluid from tissues, it helps prevent edema (swelling) and maintains the optimal volume of blood. This function is particularly important in areas such as the limbs and organs where excess fluid buildup could disrupt normal function.
Overall, the lymphatic system is essential for overall health, supporting both the immune system and fluid balance in the body. Understanding its structure and function helps highlight its importance in protecting the body from disease and ensuring the efficient functioning of bodily systems.
Understanding Blood Volume and Its Control
The volume of blood in the body is a critical factor for maintaining normal circulatory function. It affects blood pressure, tissue perfusion, and the delivery of oxygen and nutrients throughout the body. Proper regulation of blood volume ensures that the cardiovascular system operates efficiently, particularly in response to changes in physical activity, posture, and hydration levels.
Blood volume is not constant but fluctuates in response to various physiological conditions. Factors such as fluid intake, blood loss, and kidney function can all influence the total amount of blood circulating within the body. The balance between fluid intake, absorption, and elimination plays a significant role in maintaining this dynamic equilibrium.
Regulatory Mechanisms for Blood Volume
Several systems work together to regulate blood volume, primarily through the control of fluid balance. These mechanisms involve the kidneys, blood vessels, hormones, and the heart.
- Kidneys: The kidneys filter blood, regulate the amount of water and solutes excreted, and control the balance of sodium, which directly affects blood volume. When the body needs to conserve fluid, the kidneys reduce urine output, increasing blood volume. Conversely, excessive fluid intake leads to increased urine production, reducing blood volume.
- Hormones: Hormonal signals such as antidiuretic hormone (ADH) and aldosterone help regulate fluid retention and sodium levels. ADH prompts the kidneys to retain water, while aldosterone promotes sodium retention, which indirectly helps to retain water and maintain blood volume.
- Blood Vessels: The constriction or dilation of blood vessels also influences blood volume. When blood vessels constrict, the volume of blood in the circulatory system can increase due to the reduced space for the blood to flow. Dilation of blood vessels can lead to a reduction in blood volume within the system, influencing overall pressure and circulation.
- Heart: The heart plays a pivotal role in circulating blood, and its function is influenced by blood volume. A decrease in blood volume can lead to a decrease in cardiac output, while an increase in blood volume places additional strain on the heart to pump effectively.
Impact of Blood Volume on Circulatory Health
Maintaining an appropriate blood volume is crucial for overall cardiovascular health. Low blood volume (hypovolemia) can result in a decrease in blood pressure and insufficient oxygen delivery to tissues, leading to symptoms such as dizziness, weakness, or shock. Conversely, excessive blood volume (hypervolemia) can increase blood pressure, placing stress on the heart and blood vessels and potentially leading to conditions like heart failure or edema.
Adaptations to Changes in Blood Volume
The body continuously adjusts its blood volume in response to various stimuli. For example, during physical exercise, blood volume temporarily increases due to fluid retention and the redistribution of blood to active muscles. In cases of dehydration or blood loss, compensatory mechanisms such as the release of hormones and adjustments in kidney function help restore normal blood volume.
In conclusion, blood volume regulation is a dynamic process that relies on the coordinated actions of the kidneys, hormones, blood vessels, and heart. Proper understanding of these mechanisms is crucial for comprehending how the body maintains homeostasis and responds to changes in internal and external environments.
Autonomic Nervous System and Cardiovascular Control
The body’s ability to regulate vital functions, such as heart rate and blood pressure, is influenced by the complex interplay between different control systems. One of the most important contributors to this regulation is the autonomic nervous system, which adjusts the function of the heart and blood vessels in response to changes in internal and external conditions. This system operates largely unconsciously, ensuring that the body maintains homeostasis without direct conscious input.
Comprised of two major branches, the autonomic nervous system plays a central role in managing both the speed and strength of heartbeats, as well as the dilation and constriction of blood vessels. Through its actions, the system helps the body adapt to physical activity, stress, and changes in posture, ensuring adequate blood flow and oxygen delivery to tissues.
Key Components of Autonomic Control
The autonomic nervous system consists of two primary branches: the sympathetic and parasympathetic systems. Each has distinct effects on the heart and blood vessels.
- Sympathetic Nervous System: Often referred to as the “fight or flight” system, the sympathetic branch increases heart rate, the force of heart contractions, and causes the blood vessels to constrict. This prepares the body for physical exertion or stress by redirecting blood to vital organs like the muscles and brain, while reducing blood flow to less critical areas.
- Parasympathetic Nervous System: In contrast, the parasympathetic system promotes relaxation and recovery by decreasing heart rate and promoting vasodilation (widening of blood vessels). This system is primarily active when the body is at rest, ensuring efficient energy conservation and facilitating digestion and recovery processes.
Regulation of Heart Rate and Blood Pressure
Heart rate and blood pressure are controlled by dynamic feedback mechanisms that are sensitive to both internal and external changes in the body. The autonomic nervous system is central to this regulation, responding rapidly to fluctuations in factors like physical activity, emotional stress, and changes in body position.
- Heart Rate Regulation: The sympathetic nervous system accelerates heart rate by releasing norepinephrine, which binds to receptors in the heart, increasing the speed of electrical impulses and the overall rate of contractions. Conversely, the parasympathetic nervous system slows the heart rate by releasing acetylcholine, which works to decrease electrical activity in the heart.
- Blood Pressure Control: Blood pressure is influenced by the tone of the blood vessels and the volume of blood pumped by the heart. The sympathetic system constricts blood vessels, increasing peripheral resistance and raising blood pressure, while the parasympathetic system causes dilation of blood vessels, leading to a reduction in blood pressure.
Through this continuous modulation, the autonomic nervous system ensures that the body can respond to varying demands for oxygen and nutrients, while maintaining a stable internal environment. Whether in times of stress or relaxation, the balance between these two systems allows the heart and blood vessels to function efficiently under a wide range of conditions.
Cardiovascular Adaptations to Exercise
During physical activity, the body undergoes various changes to meet the increased demands for oxygen and nutrients by muscles and other tissues. These adjustments occur within the heart, blood vessels, and blood volume to ensure that energy supply is optimized. The ability of the heart and circulatory system to adapt to these demands is essential for improving performance and endurance. Regular exercise leads to both short-term responses and long-term structural changes that enhance the efficiency of the body’s delivery systems.
Immediate Responses to Physical Activity
As soon as exercise begins, several mechanisms are activated to increase blood flow and oxygen delivery to active muscles. These responses are immediate and critical for maintaining performance throughout the activity.
- Heart Rate Increase: The heart rate rises to pump more blood per minute, increasing the amount of oxygen transported to the muscles. This is achieved by signals from the sympathetic nervous system, which accelerates heart rate and contractility.
- Blood Vessel Dilation: In response to physical activity, blood vessels in the working muscles dilate (vasodilation), allowing more blood to flow through them. At the same time, vessels to non-essential areas constrict to prioritize blood flow to where it is most needed.
- Increased Cardiac Output: The combination of higher heart rate and stronger heart contractions results in an increased cardiac output, meaning the heart pumps more blood per minute to meet the demands of the body during exercise.
Long-Term Adaptations to Regular Exercise
With consistent exercise, the body undergoes structural changes that improve its ability to handle physical exertion, resulting in enhanced performance over time.
- Improved Stroke Volume: Regular training leads to an increase in stroke volume–the amount of blood pumped by the heart with each beat. This allows the heart to deliver more blood per beat, improving overall efficiency and reducing the need for excessively high heart rates during activity.
- Reduced Resting Heart Rate: Over time, the heart becomes more efficient, and its resting rate decreases. This is a sign of a well-conditioned heart that requires fewer beats to supply the body with sufficient blood at rest.
- Enhanced Blood Volume: Chronic exercise increases the total volume of blood in the body. This enables the cardiovascular system to transport more oxygen and nutrients, supporting prolonged physical activity.
These adaptations contribute not only to improved endurance but also to overall health benefits. Regular exercise enhances the efficiency of oxygen delivery, promotes better circulation, and can lower the risk of cardiovascular diseases by strengthening the heart and blood vessels.
Common Cardiovascular Pathologies and Disorders
The heart and blood vessels are susceptible to a variety of conditions that can impair their function. These disorders can affect the efficiency of circulation, oxygen delivery, and overall health. Understanding these common issues is essential for identifying symptoms, diagnosing conditions, and implementing effective treatments. These ailments often result from lifestyle factors, genetic predispositions, or other underlying health issues, and their impact can range from mild discomfort to life-threatening complications.
- Hypertension: High blood pressure is one of the most prevalent conditions, where the force of blood against the artery walls is consistently too high. This can lead to damage to the heart and other organs if left untreated. Risk factors include obesity, lack of exercise, smoking, and excessive salt intake.
- Coronary Artery Disease: This condition occurs when the arteries that supply blood to the heart muscle become narrowed or blocked by plaque buildup, limiting blood flow. It can result in chest pain, heart attacks, or other severe complications.
- Atherosclerosis: A progressive condition where the arteries become stiff and narrowed due to the accumulation of fatty deposits. This reduces the efficiency of blood flow and increases the risk of heart attack, stroke, and other serious health problems.
- Heart Failure: When the heart is unable to pump blood effectively, it can lead to heart failure. This can occur due to weakened heart muscle, valve problems, or high blood pressure over time. Symptoms may include fatigue, shortness of breath, and fluid retention.
- Arrhythmias: Abnormal heart rhythms, such as atrial fibrillation or ventricular tachycardia, can cause the heart to beat too fast, too slow, or erratically. These disturbances can affect the heart’s ability to pump blood efficiently and may lead to dizziness, fainting, or even stroke.
- Valvular Disorders: Heart valve problems, such as stenosis or regurgitation, occur when the valves in the heart do not open or close properly, disrupting normal blood flow. These conditions can lead to symptoms like chest pain, fatigue, and shortness of breath.
These conditions often have overlapping risk factors and may require ongoing medical management, including medication, lifestyle changes, or surgical intervention. Early detection and treatment are crucial to prevent severe complications and improve quality of life.