Generic Physical Exam Form for Healthcare Use
In healthcare settings, the ability to collect comprehensive and accurate patient information is essential for effective diagnosis and treatment. Structured documentation plays a key role in ensuring that all critical data is captured during a patient evaluation. These templates help healthcare providers systematically assess various health parameters, ensuring that no important detail is overlooked.
Standardized documentation provides a uniform approach to patient assessments, making it easier to compare results over time and across different providers. By utilizing these tools, professionals can improve consistency and reliability in their evaluations.
Whether used in routine check-ups or more specialized consultations, these tools allow for streamlined data collection and improved patient care. Their role extends beyond just recording information; they also facilitate communication between medical staff and contribute to better decision-making in patient management.
Overview of Health Evaluation Templates
Health evaluation templates are essential tools used by healthcare providers to document key aspects of a patient’s health during assessments. These tools offer a structured approach, ensuring that vital information is recorded consistently and thoroughly. They serve as a framework for organizing patient data, which aids in accurate diagnosis and effective treatment planning.
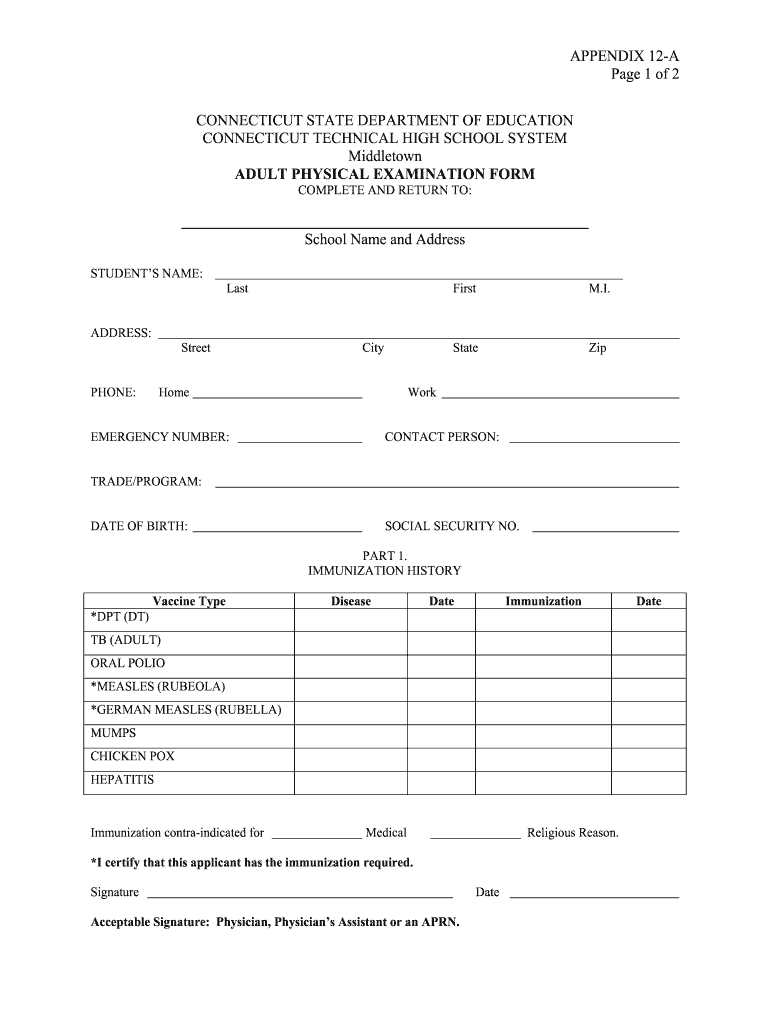
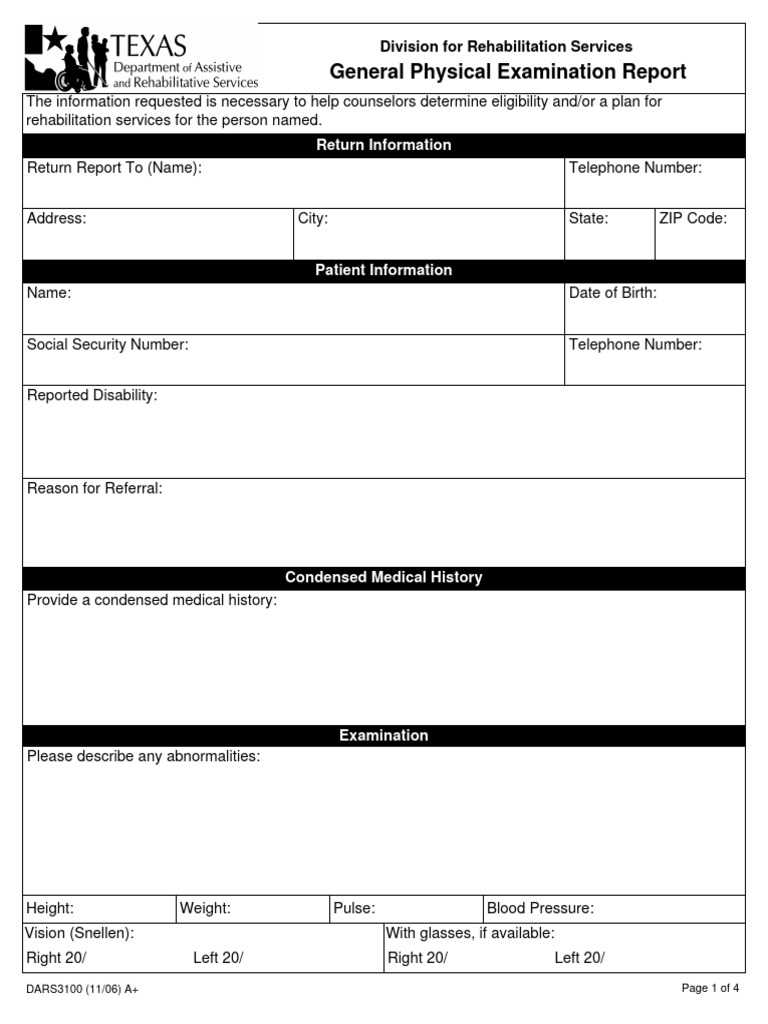
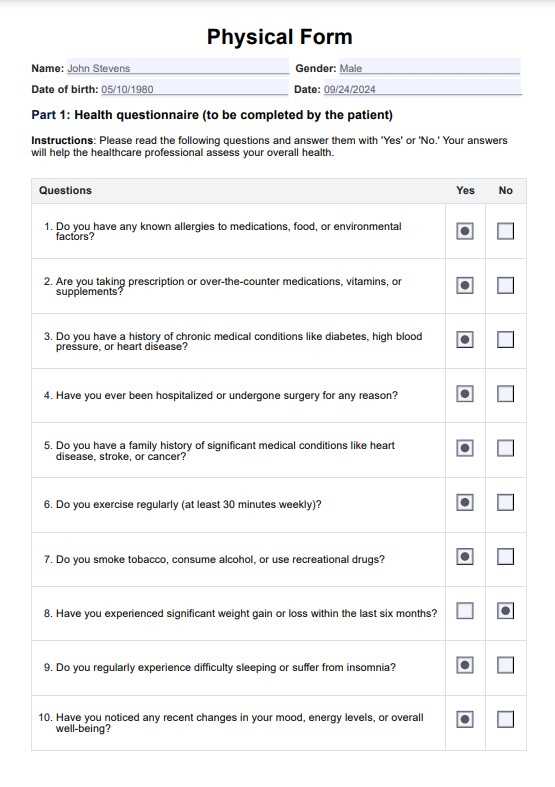
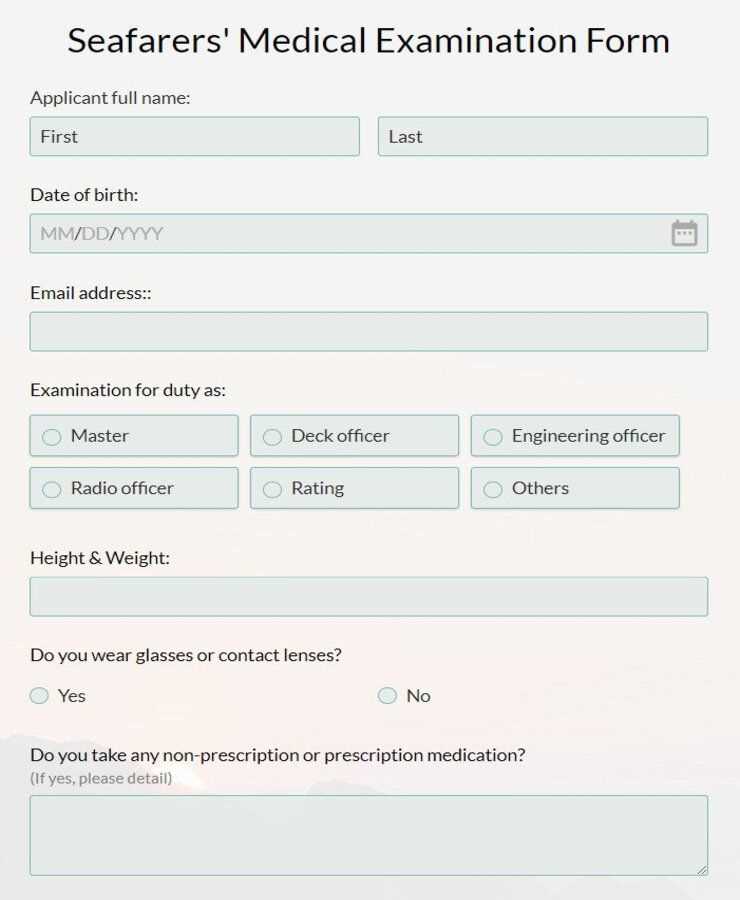
Typically, these templates are designed to capture a wide range of health indicators, including:
- Vital signs such as blood pressure, heart rate, and temperature
- Physical attributes, like weight, height, and body mass index (BMI)
- Systems review, covering cardiovascular, respiratory, and neurological functions
- Patient medical history, including past illnesses and family history
- Current medications and allergies
The purpose of these tools extends beyond simple record-keeping. By standardizing the evaluation process, they help minimize errors, improve workflow efficiency, and promote better communication among medical staff. These templates also enable quick access to important information, ensuring that practitioners can make informed decisions at the point of care.
Purpose of Health Assessment Tools
Health assessment tools are crucial for capturing and organizing essential patient information during medical evaluations. Their primary function is to ensure that healthcare providers have a consistent, structured method for documenting critical health data. These documents enable professionals to assess a patient’s current condition and track changes over time, leading to more accurate diagnoses and tailored treatment plans.
Enhancing Accuracy and Consistency
By providing a standardized format, these tools reduce the likelihood of missed details, ensuring that all aspects of the patient’s health are reviewed. This consistency not only supports more reliable medical records but also improves patient care by preventing errors and enhancing communication among medical staff.
Facilitating Informed Decision-Making
Incorporating detailed information into each evaluation helps healthcare providers make well-informed decisions. Having all relevant data at hand allows for quick, accurate assessments, which is especially important in urgent care settings. In this way, these tools directly contribute to the efficiency and effectiveness of patient management.
Key Components of Health Assessment Tools
Health evaluation documents are designed to capture a wide range of essential data that provides a comprehensive picture of a patient’s health. These tools are structured to include various sections, each focusing on specific aspects of the patient’s condition. The goal is to ensure that no critical information is overlooked and that healthcare providers have all the necessary details to make informed decisions.
Some of the key components typically found in these tools include:
- Patient Identification: Basic details such as name, age, gender, and medical history
- Vital Signs: Measurements like blood pressure, heart rate, temperature, and respiratory rate
- Physical Measurements: Information on height, weight, BMI, and other body metrics
- Systems Review: A thorough evaluation of different body systems such as cardiovascular, respiratory, and neurological health
- Medical History: Details of past illnesses, surgeries, allergies, and medications
Each of these sections plays a crucial role in helping healthcare providers track the patient’s health over time and identify any changes or issues that require attention. By systematically organizing this information, the document ensures consistency in evaluations and allows for easier comparison between visits or different healthcare providers.
How to Customize Health Assessment Tools for Patients
Customizing health evaluation documents for individual patients ensures that their unique medical needs are accurately captured during an assessment. Tailoring these tools allows healthcare providers to focus on relevant health aspects, making the evaluation process more efficient and effective. Personalization also improves the quality of care by addressing specific concerns and medical histories.
Here are several ways to adjust these documents for a particular patient:
- Incorporate Relevant Medical History: Ensure the patient’s past conditions, surgeries, and family history are included, especially if they affect current health assessments.
- Adjust Sections Based on Specialty: For example, if the patient is seeing a cardiologist, emphasize cardiovascular measurements, while a pediatric evaluation might focus more on growth and development.
- Highlight Current Concerns: Include questions or sections that address the specific issues the patient is facing during that visit, such as pain levels, symptoms, or mental health screenings.
- Use Clear and Patient-Friendly Language: Adapt the terminology to be easily understood by the patient, especially in sections where self-reporting is required.
By customizing these tools, healthcare providers can enhance patient engagement and ensure that assessments are thorough, relevant, and aligned with individual healthcare needs.
Benefits of Using Standardized Tools
Standardizing health assessment tools offers numerous advantages that improve the efficiency, accuracy, and consistency of patient evaluations. These tools provide a uniform structure, ensuring that all relevant data is captured in a clear and organized manner. By using standardized methods, healthcare providers can streamline their workflow and improve communication across teams.
Improved Accuracy and Consistency
Standardized templates help minimize errors and reduce variability in how data is recorded, ensuring that each assessment is thorough and accurate. This consistency is crucial for maintaining reliable medical records, which in turn leads to better patient care and decision-making.
Enhanced Efficiency and Productivity
These tools save time by guiding healthcare providers through the evaluation process with predefined sections and prompts. The ability to quickly capture key information allows practitioners to focus more on patient care rather than on figuring out what to record or how to document it.
- Time-saving: Reduces the need for repeated data collection or unnecessary steps in the process.
- Uniformity: Ensures consistency in assessments, especially across different providers or locations.
- Better Coordination: Facilitates communication between healthcare professionals by providing a common structure for patient records.
Overall, the use of standardized evaluation tools leads to more streamlined healthcare delivery, fostering a more efficient and effective approach to patient management.
Importance of Accurate Health Documentation
Accurate and comprehensive medical records are essential for effective patient care and clinical decision-making. These records provide healthcare providers with a clear history of a patient’s health, enabling them to track progress, identify trends, and make informed decisions. Without precise documentation, critical information may be overlooked, leading to misdiagnosis, delayed treatment, or unnecessary tests.
Ensuring Continuity of Care
Accurate health records are crucial for ensuring continuity of care, especially when multiple healthcare providers are involved. These records allow for seamless transitions between providers and ensure that all team members are informed about the patient’s history, treatment plan, and any special needs. Inaccurate or incomplete records can lead to gaps in care, which can negatively affect patient outcomes.
Legal and Ethical Considerations
Proper documentation is not only vital for clinical reasons but also for legal and ethical purposes. In the event of disputes or audits, accurate records serve as evidence of the care provided. Moreover, maintaining clear and truthful records helps ensure compliance with healthcare regulations and protects both the patient and provider.
| Key Benefits of Accurate Documentation | Impact |
|---|---|
| Improved Patient Safety | Reduces errors and ensures the right treatments are provided at the right time. |
| Enhanced Communication | Facilitates collaboration between different healthcare providers, ensuring informed decision-making. |
| Legal Protection | Serves as documentation in case of legal inquiries, proving that appropriate care was given. |
| Better Decision-Making | Helps providers make informed choices based on a comprehensive understanding of the patient’s history. |
Ultimately, accurate health documentation serves as the foundation for effective medical care, legal protection, and efficient healthcare operations.
Types of Information Collected in Assessment Tools
Health assessment tools are designed to gather a wide range of essential information that helps healthcare providers understand a patient’s overall well-being. These tools systematically collect data across various areas of health, ensuring that important details are documented for accurate diagnosis, treatment planning, and follow-up care. The data collected provides a comprehensive snapshot of a patient’s current condition and medical history.
The types of information typically gathered include:
| Category | Details Collected |
|---|---|
| Personal Information | Name, age, gender, contact details, and emergency contacts |
| Vital Signs | Blood pressure, heart rate, temperature, respiratory rate |
| Medical History | Previous illnesses, surgeries, allergies, family health history |
| Current Medications | List of prescribed and over-the-counter medications, dosages, and duration |
| Physical Measurements | Height, weight, body mass index (BMI), waist circumference |
| Systems Review | Details about cardiovascular, respiratory, neurological, and other systems |
By systematically collecting and organizing this information, healthcare professionals are better equipped to evaluate a patient’s overall health, identify risk factors, and make informed decisions regarding their care. This approach also ensures that no critical data is missed during the assessment process.
How to Improve Patient Assessments
Enhancing the quality of patient assessments is crucial for accurate diagnosis, effective treatment, and better healthcare outcomes. The process of gathering patient information should be thorough, clear, and tailored to the individual’s unique needs. By focusing on key areas, healthcare providers can gain deeper insights into a patient’s health and identify potential issues early.
Here are several strategies to improve the quality of patient assessments:
- Focus on Comprehensive Data Collection: Ensure that all relevant areas of health are covered, including medical history, lifestyle factors, and mental well-being, to gain a holistic view of the patient.
- Encourage Open Communication: Foster a comfortable environment where patients feel confident sharing personal health concerns. Active listening and empathy are key to understanding their needs fully.
- Regularly Update Health Records: Keep patient records current and accurate. This ensures that any changes in health status or new conditions are promptly identified and addressed.
- Incorporate Technology: Utilize digital tools and health tracking systems to streamline data collection and enhance the accuracy of assessments. These technologies can help in tracking trends over time and improving decision-making.
- Personalize the Assessment Process: Tailor the assessment to the patient’s age, condition, and risk factors. For example, a pediatric evaluation will differ from an assessment for an elderly patient with chronic conditions.
By implementing these strategies, healthcare providers can ensure that assessments are more accurate, efficient, and patient-centered, ultimately leading to better care and improved health outcomes.
Legal Considerations in Medical Documents
When collecting and recording patient information, healthcare providers must ensure that all documents meet legal requirements to protect both the patient and the provider. Proper documentation not only serves medical purposes but also helps safeguard against potential legal disputes. Accurate and detailed records are crucial in demonstrating that appropriate care has been provided and that the patient’s rights have been respected.
Confidentiality and Privacy
One of the primary legal considerations is maintaining the confidentiality of patient information. Healthcare providers must adhere to regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. or other local data protection laws to ensure that patient details are not disclosed without consent. This includes secure handling, storage, and transmission of medical records.
Informed Consent and Documentation
Informed consent is another critical legal element. Healthcare providers must obtain explicit consent from patients before proceeding with any assessments or treatments, and this consent must be properly documented. The documentation should clearly outline the nature of the procedure, the risks involved, and the patient’s agreement to proceed. This protects both the patient’s autonomy and the provider’s legal standing.
In summary, adhering to legal guidelines in medical documentation ensures patient confidentiality, protects healthcare providers from legal risks, and supports the overall integrity of the healthcare process.
Ensuring Confidentiality in Patient Records
Protecting the privacy of patient information is a fundamental aspect of healthcare practice. Confidentiality in patient records not only preserves trust between healthcare providers and patients but also complies with legal and ethical standards. Safeguarding sensitive data ensures that personal health information is only accessed by authorized individuals and is not disclosed without the patient’s consent.
Implementing Secure Storage Systems
One of the most effective ways to maintain confidentiality is by using secure storage systems for patient data. This includes both physical and digital methods of storing medical records. For digital records, encryption and password protection should be standard procedures to prevent unauthorized access. For physical records, locked cabinets and restricted access to office spaces can significantly reduce the risk of breaches.
Training Staff on Confidentiality Practices
Ensuring that all healthcare personnel understand the importance of maintaining confidentiality is crucial. Regular training on data protection protocols, privacy regulations, and the consequences of breaches helps reinforce the responsibility healthcare workers have in protecting patient information. Additionally, establishing clear guidelines for sharing patient data within the organization and with external parties is essential for compliance.
By integrating these measures into everyday healthcare practices, organizations can ensure that patient information remains confidential and secure, fostering trust and safeguarding the integrity of the healthcare system.
Common Mistakes in Filling Out Medical Documents
Accurate completion of medical documentation is crucial for effective healthcare delivery. However, there are common mistakes that often occur during the process, which can lead to misinterpretation, delays in care, or legal complications. Recognizing these errors and understanding how to avoid them can improve the overall quality and accuracy of patient records.
Incomplete or Missing Information
One of the most frequent mistakes is leaving sections of the document incomplete. Missing details such as patient contact information, medical history, or vital signs can hinder proper diagnosis and treatment planning. It’s important to ensure that all fields are thoroughly filled out, and any relevant information is included to provide a full picture of the patient’s health.
Illegible Handwriting or Typographical Errors
Illegible handwriting or typographical errors can create confusion and lead to misunderstandings. Whether it’s in paper-based or electronic documents, unclear writing can prevent healthcare professionals from accurately interpreting patient data. Using clear, legible handwriting, or opting for typed entries where possible, can significantly reduce these types of mistakes.
By addressing these common issues, healthcare providers can enhance the quality of their documentation, ensuring that it accurately reflects the patient’s health status and that necessary actions can be taken in a timely manner.
Best Practices for Medical Documentation
Effective and accurate medical documentation is essential for providing high-quality care. Proper record-keeping ensures that all relevant patient information is clearly captured, making it easier for healthcare providers to make informed decisions and coordinate care. Following best practices for documenting patient assessments can reduce errors, improve communication, and support legal and regulatory compliance.
Maintain Consistency and Clarity
One of the key aspects of good documentation is consistency. Use standardized terminology and formats to ensure that information is easy to understand and compare. This helps avoid confusion and ensures that all healthcare professionals reviewing the document are on the same page. Clear and concise language is also essential–avoiding jargon or vague descriptions ensures that the document accurately reflects the patient’s condition and treatment plan.
Include All Relevant Information
Complete documentation should include all pertinent details about the patient’s health, including history, current conditions, and any diagnostic or treatment procedures. Don’t omit important data or skip sections, as incomplete records can lead to miscommunication and potential risks to the patient’s care. Additionally, it’s important to document any patient concerns or symptoms in their own words, as this can provide valuable insight into their condition.
By adhering to these best practices, healthcare providers can ensure that their documentation is accurate, comprehensive, and useful for ongoing patient care and legal protection.
How to Train Staff on Using Medical Documentation
Training healthcare staff to accurately use medical documentation is crucial to maintaining high-quality patient care and compliance with legal requirements. Effective training ensures that every team member understands the process, follows best practices, and avoids common mistakes when recording patient information. Proper guidance can also help increase efficiency and reduce errors in healthcare settings.
Develop Clear Training Materials
Training materials should be clear, easy to follow, and tailored to the specific needs of your healthcare team. These materials should include examples of properly filled-out documents, instructions on what to record, and guidelines for handling sensitive patient information. Visual aids, such as templates or checklists, can be particularly helpful in illustrating how to fill out each section of the documentation accurately.
Conduct Hands-On Training Sessions
Hands-on training allows staff to practice using the documentation in a controlled environment. Conducting mock exercises where staff complete sample records can help identify areas where they may need additional guidance. Role-playing scenarios with patient interactions also provide a practical learning experience, ensuring that the team is comfortable and confident with the process before they work with real patient data.
| Training Component | Details |
|---|---|
| Documentation Guidelines | Provide written instructions and best practices for filling out documents accurately. |
| Interactive Exercises | Use mock scenarios and sample records to practice the documentation process. |
| Confidentiality and Compliance | Teach staff the importance of maintaining patient privacy and following legal requirements. |
Regular refresher courses should also be scheduled to ensure that all staff members remain up-to-date on documentation protocols and any changes in regulatory requirements. This ongoing education will help maintain the accuracy and consistency of medical records throughout your practice.
Integrating Digital Documentation in Healthcare
The shift towards digital solutions in healthcare has transformed how patient information is collected and managed. By adopting electronic documentation tools, healthcare providers can streamline the recording process, improve accessibility, and reduce the risk of errors. The integration of digital documentation systems offers a more efficient way to handle patient data, making it easier to store, retrieve, and share information securely across various platforms.
Benefits of Digital Documentation
Digital documentation systems offer numerous advantages over traditional paper-based methods. These include:
- Improved Accuracy: Automated systems reduce human error by guiding users through the correct fields and ensuring that all necessary data is entered.
- Faster Data Entry: Electronic systems can auto-fill certain fields, speeding up the documentation process and allowing healthcare professionals to focus more on patient care.
- Enhanced Accessibility: Patient records can be accessed by authorized personnel from any location, improving collaboration among healthcare teams.
- Data Security: Digital tools offer encryption and secure storage, ensuring patient information is protected from unauthorized access.
Challenges of Digital Integration
Despite the many benefits, integrating digital documentation systems can pose challenges, such as:
- Initial Setup Costs: Transitioning to digital systems may require significant upfront investment in software, hardware, and training.
- Staff Training: Healthcare professionals need to be trained on how to use new digital systems effectively, which can take time and resources.
- Data Privacy Concerns: Ensuring compliance with healthcare regulations, such as HIPAA, is crucial to protecting patient privacy in the digital space.
Overall, the transition to digital documentation in healthcare can improve the quality and efficiency of care delivery, provided the implementation is well-planned and properly executed. With ongoing advancements in technology, digital systems are becoming an increasingly important tool in modern healthcare practices.
How Documents Support Medical Decision-Making
Medical documentation plays a crucial role in assisting healthcare professionals in making informed decisions. By providing a structured way to capture patient information, these records help clinicians assess symptoms, track progress, and determine the most appropriate course of treatment. Whether in digital or paper form, these documents serve as a valuable tool to guide decisions, ensuring that nothing critical is overlooked.
Key Ways Documents Influence Decision-Making
Medical documentation impacts decision-making in several important ways:
- Comprehensive Overview: A well-organized document provides a clear and detailed history of a patient’s health, offering essential context for diagnoses and treatment plans.
- Accurate Tracking of Symptoms: By recording changes in symptoms or conditions over time, healthcare providers can make data-driven adjustments to treatment strategies.
- Informed Choices: Documentation allows professionals to evaluate multiple factors–such as medical history, current medications, and lab results–leading to more precise decisions.
- Clear Communication: These documents ensure that all team members involved in patient care have access to the same information, fostering collaboration and reducing the risk of errors.
Supporting Evidence-Based Practice
Incorporating well-structured documentation into clinical practice supports evidence-based decision-making. By systematically organizing relevant information, medical records allow healthcare providers to apply clinical guidelines, best practices, and research findings to each patient’s unique situation. This leads to:
- Standardization: Healthcare teams can align on treatment protocols, ensuring consistency in care.
- Better Outcomes: Access to historical data and trends aids in forecasting potential complications or improvements, enabling timely interventions.
- Reduced Mistakes: Structured records limit human error by ensuring that key details are not overlooked.
Ultimately, documents act as a foundation for sound decision-making, enabling healthcare providers to offer high-quality, patient-centered care while reducing risk and enhancing efficiency.
Maintaining Consistency in Patient Evaluations
Consistency in patient assessments is essential for providing reliable and accurate healthcare. When medical evaluations are performed in a uniform manner, it ensures that healthcare providers can track a patient’s progress over time and make well-informed decisions. A structured approach helps to minimize errors, avoid confusion, and deliver a higher standard of care.
The Role of Standardized Procedures
Standardized evaluation methods ensure that each patient is assessed using the same criteria, allowing for:
- Reliable Comparisons: By following the same process, healthcare professionals can compare results across appointments, highlighting any changes in a patient’s condition.
- Efficient Documentation: Using consistent methods for recording information simplifies data entry and ensures that all critical factors are captured in the same way each time.
- Fewer Discrepancies: A uniform approach reduces the likelihood of discrepancies in assessments, making it easier to identify any potential issues or deviations from expected outcomes.
Training and Best Practices for Consistency
To maintain consistency, it is crucial to train healthcare providers on best practices for evaluations. This includes:
- Clear Protocols: Having established guidelines and protocols helps staff to follow a uniform process during every patient assessment.
- Regular Reviews: Periodically reviewing records and assessments ensures that any inconsistencies can be identified and corrected in a timely manner.
- Continuous Education: Keeping staff updated on the latest healthcare practices and technologies encourages adherence to best practices and consistency in evaluations.
Ultimately, maintaining consistency in patient assessments contributes to better care quality, improves patient outcomes, and enhances the overall effectiveness of healthcare teams.
Updating and Revising Health Assessment Documents
Regular updates and revisions of assessment documents are essential to ensure they remain effective, accurate, and compliant with the latest medical standards. As healthcare practices evolve, it is crucial to refine and adjust evaluation tools to better capture relevant patient information and support decision-making. This process helps improve the quality of care and ensures that medical professionals have the most up-to-date resources at their disposal.
Reasons for Revising Medical Evaluation Tools
There are several reasons why revising evaluation documents is necessary:
- Medical Advancements: New research, treatments, and diagnostic techniques require updated documentation to reflect current knowledge and practices.
- Regulatory Changes: Laws and regulations regarding patient care, privacy, and data collection may change, necessitating adjustments to ensure compliance.
- Improved Accuracy: Feedback from healthcare providers can reveal areas where the current document may lack clarity or fail to capture important data, prompting revisions for better accuracy.
Best Practices for Updating Health Documents
When revising evaluation tools, it is important to follow a structured approach:
- Review Feedback: Gather input from healthcare providers who use the documents regularly. Their practical experience can highlight areas for improvement.
- Test New Versions: Before implementing revisions across the board, pilot the updated document with a small group of users to ensure it is clear, comprehensive, and easy to use.
- Regular Audits: Periodically audit existing assessment tools to identify outdated sections or unnecessary content that can be streamlined or eliminated.
- Ensure Flexibility: Make sure the revised documents remain adaptable to different patient needs, including special considerations for various demographics or conditions.
By regularly updating and revising health assessment tools, healthcare organizations can maintain the accuracy and effectiveness of their evaluation processes, leading to improved patient care and operational efficiency.