ACLS Pre Course Assessment Answers for Your Certification
In the process of obtaining your certification for advanced emergency care, understanding essential medical concepts and protocols is crucial. The preparation phase plays a key role in ensuring you’re ready for real-life scenarios that require quick decision-making and precise actions. This phase focuses on building a strong foundation in critical care techniques and understanding the specific steps involved in life-saving procedures.
To succeed in this preparatory phase, it’s important to familiarize yourself with key procedures, medical responses, and effective teamwork during emergencies. The questions posed during this stage aim to test your knowledge and ability to apply guidelines in realistic situations. By reviewing the material thoroughly, you will not only increase your confidence but also ensure you’re equipped with the necessary skills to handle high-pressure situations effectively.
Focus on critical areas such as cardiac arrest management, airway interventions, and arrhythmia recognition. Mastering these topics will help you navigate the complexities of the exam and enhance your overall performance. Preparation is more than just memorizing facts–it’s about developing a comprehensive understanding of the concepts that will ultimately save lives in emergency medical situations.
ACLS Pre Course Assessment Overview
As part of your preparation for advanced life support certification, the initial phase involves testing your understanding of critical medical concepts. This stage is designed to evaluate your readiness by focusing on key procedures and protocols necessary for handling emergencies. It helps identify areas where further review is needed and ensures you are prepared for more complex scenarios during practical training.
The primary goal of this evaluation is to assess your foundational knowledge in several essential topics. This includes everything from recognizing life-threatening arrhythmias to understanding how to perform effective resuscitation techniques. Successful completion of this stage indicates that you are well-prepared to advance in your training and certification process.
- Recognizing and managing cardiac arrest
- Understanding advanced airway techniques
- Identifying and treating arrhythmias
- Administering emergency medications properly
- Following correct resuscitation protocols in high-pressure situations
By familiarizing yourself with these areas and reviewing the concepts carefully, you will enhance your chances of success in subsequent training sessions and ensure that you’re fully equipped for emergency situations. The evaluation process is a critical step that lays the groundwork for further learning and ultimately helps you provide the best possible care during life-saving interventions.
Importance of the Pre Course Assessment
Before advancing to more hands-on training in emergency medical procedures, it’s crucial to evaluate your current knowledge and understanding of essential topics. This initial review serves as a foundation for ensuring that you are prepared to handle high-pressure situations effectively. It helps identify any gaps in knowledge that may need further attention, setting the stage for more advanced training.
By taking part in this early evaluation, you can focus your efforts on the most important areas of care and improve your ability to apply life-saving procedures correctly. It also provides insight into your familiarity with emergency protocols, enabling you to approach the practical aspects of the program with greater confidence and precision.
This phase is not just a test but a vital tool for reinforcing the core concepts and techniques that will be used in real-world emergencies. It ensures that when it comes time for actual intervention, you have the necessary skills and theoretical knowledge to act swiftly and competently under pressure.
Key Topics Covered in ACLS Assessment
The initial evaluation focuses on a range of critical medical topics that are essential for effective emergency care. These areas form the backbone of any advanced intervention and are designed to test your understanding of the most urgent procedures used in life-threatening situations. Each topic plays a vital role in ensuring that you can respond accurately and efficiently when faced with medical emergencies.
Cardiac Arrest and Resuscitation Procedures
One of the primary areas covered is cardiac arrest management, where you’ll need to demonstrate your knowledge of how to recognize and treat patients experiencing sudden cardiac arrest. This includes performing high-quality chest compressions, managing defibrillation, and administering appropriate medications. Understanding when and how to apply each intervention is crucial for increasing survival rates.
Airway Management and Ventilation Techniques
Effective airway management is another critical area, focusing on techniques to maintain a clear airway and ensure adequate ventilation in a variety of emergency situations. You’ll be assessed on your knowledge of various methods for securing an airway, including mechanical ventilation and manual techniques, to prevent complications and support respiratory function.
These topics provide a comprehensive overview of the life-saving procedures you’ll need to master in order to handle serious medical emergencies with confidence and skill. Mastering these concepts ensures that you are prepared for practical training and eventual certification in advanced emergency care.
How to Approach the Assessment Questions
When preparing for an evaluation focused on advanced medical protocols, it’s essential to approach each question with a clear, methodical mindset. This ensures that you not only recall the necessary information but also understand how to apply it in real-world situations. Proper preparation and strategy can greatly enhance your performance and confidence throughout the evaluation process.
First, take time to carefully read each question, ensuring that you fully understand what is being asked. Often, the wording can be tricky, and it’s easy to overlook important details. Identifying keywords and focusing on the main idea of the question will help you select the correct response.
Next, rely on your understanding of core principles. Many questions will test your ability to apply theoretical knowledge to practical scenarios. Think about the steps involved in each procedure and how they align with emergency care protocols. Break down complex questions by considering the sequence of actions and the desired outcomes. This methodical approach will allow you to navigate even the more challenging questions with ease.
Additionally, be aware of common distractors–incorrect options that seem plausible but are not aligned with best practices. These can often be ruled out by focusing on your understanding of evidence-based practices and proven guidelines. The goal is not just to remember facts, but to think critically about the most effective response to each scenario.
Understanding Cardiac Arrest Management
Managing a cardiac arrest situation requires precise knowledge of emergency protocols and the ability to act swiftly. In these high-pressure moments, every second counts, and effective intervention can significantly improve the chances of survival. A clear understanding of the steps involved–from recognizing the condition to performing resuscitation–is essential for providing immediate care to those in need.
First, it’s crucial to recognize the signs of a cardiac arrest. The patient may suddenly collapse, lose consciousness, and stop breathing or have abnormal breathing. Immediate recognition leads to faster response, which is critical for restoring circulation and preventing brain damage.
Once identified, the next step is performing chest compressions. High-quality chest compressions are essential to maintain blood flow to vital organs. Proper depth, rate, and minimizing interruptions are key elements of effective compression. Alongside this, defibrillation should be considered if appropriate, as it can restore a normal rhythm in certain types of arrhythmias.
Administering the right medications, monitoring vital signs, and coordinating with other team members during resuscitation are also crucial aspects of managing cardiac arrest. Effective teamwork and communication in these situations can make a significant difference in outcomes. Post-cardiac arrest care involves stabilizing the patient and addressing underlying causes, ensuring they receive the best possible care for recovery.
Roles of Advanced Airway Management
Effective airway management is a cornerstone of emergency care, especially when dealing with patients who are unable to maintain their own breathing. Securing the airway ensures that oxygen reaches the lungs, which is vital for survival and neurological function. Advanced techniques are used in critical situations to support, secure, and maintain a patent airway when basic methods are insufficient.
Indications for Advanced Techniques
Advanced airway management techniques are typically required when patients are unable to protect their airway, such as in cases of unconsciousness, trauma, or severe respiratory distress. Endotracheal intubation is one of the most common procedures, where a tube is inserted into the trachea to ensure an open pathway for air to reach the lungs. This is especially crucial when manual ventilation or less invasive methods cannot guarantee sufficient oxygenation.
Key Techniques in Airway Management
In addition to endotracheal intubation, other methods such as laryngeal mask airways (LMA) and supraglottic devices are used to maintain the airway in certain scenarios. These alternatives are particularly beneficial in situations where intubation may be difficult or time-consuming. Additionally, effective use of bag-valve-mask ventilation remains a critical part of airway management, especially during the initial stages of resuscitation.
Understanding the role of these techniques and knowing when to apply them is essential for ensuring that oxygen is delivered to the body and brain, preventing further complications. Advanced airway management is not just about securing the airway but also about providing ongoing ventilation to support life functions.
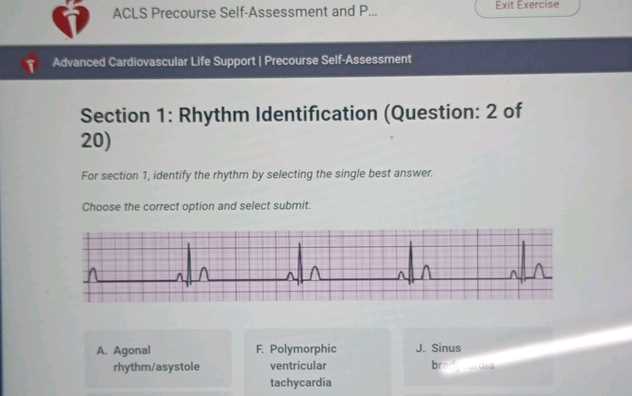
Recognizing Cardiac Arrhythmias Effectively
Identifying abnormal heart rhythms is a critical skill in emergency medical care. Cardiac arrhythmias, whether they are too fast, too slow, or irregular, can lead to life-threatening complications if not addressed promptly. Recognizing these irregularities quickly allows for timely intervention, which can greatly improve patient outcomes. Understanding the different types of arrhythmias and their corresponding electrocardiogram (ECG) patterns is essential for effective diagnosis and treatment.
Common Types of Arrhythmias
There are several types of arrhythmias, each with distinct characteristics and treatment protocols. Some of the most common arrhythmias include atrial fibrillation, ventricular tachycardia, and bradycardia. Recognizing the signs and ECG patterns associated with these conditions is vital for providing immediate care and determining the most appropriate course of action.
| Arrhythmia | ECG Features | Clinical Significance |
|---|---|---|
| Atrial Fibrillation | Irregularly irregular rhythm with no distinct P waves | Increased risk of stroke and heart failure |
| Ventricular Tachycardia | Rapid, wide QRS complexes | Can lead to cardiac arrest if untreated |
| Bradycardia | Heart rate | May cause dizziness, fainting, or shock in severe cases |
Approaching Arrhythmia Diagnosis
To effectively diagnose arrhythmias, it’s essential to monitor the patient’s symptoms and correlate them with the observed ECG patterns. Clinical signs such as chest pain, shortness of breath, or lightheadedness often accompany abnormal rhythms, making it easier to identify the underlying issue. Once recognized, the next step is determining the appropriate treatment, which may involve medications, electrical cardioversion, or other interventions depending on the severity and type of arrhythmia.
Quick and accurate recognition of cardiac arrhythmias can significantly improve patient outcomes by ensuring that the right treatment is applied as soon as possible. Consistent practice and familiarity with ECG readings are essential for developing the skills needed to identify these conditions effectively.
Common Mistakes to Avoid in the Assessment
During evaluations focused on emergency medical protocols, it is easy to make mistakes that can hinder performance or lead to incorrect conclusions. These errors often arise from misunderstandings of protocols, failure to apply best practices, or overlooking crucial details in questions. Avoiding these common pitfalls can help you achieve better results and ensure a thorough understanding of life-saving procedures.
Key Mistakes and How to Avoid Them
Recognizing common errors can help you avoid them during the evaluation process. Below are some typical mistakes and strategies for addressing them:
| Mistake | How to Avoid |
|---|---|
| Misinterpreting the Question | Carefully read each question and identify the main concept being tested before answering. Look for key phrases that guide your response. |
| Overlooking Key Steps in Procedures | Focus on the sequence of steps in medical protocols. Ensure you understand the order in which actions should be taken for optimal results. |
| Choosing Distractors | Be cautious of choices that seem plausible but are not aligned with best practices. Rely on evidence-based knowledge to guide your decisions. |
| Skipping Review of Answers | Before finalizing your responses, review all answers to ensure accuracy and completeness. Look for any inconsistencies or overlooked details. |
Ensuring Confidence and Accuracy
By identifying and avoiding these common mistakes, you will approach the evaluation process with greater confidence and accuracy. Take time to practice and review the material regularly to ensure that you are familiar with the protocols and procedures. Accurate knowledge and clear thinking during the evaluation will ensure you’re well-prepared for any scenario that may arise.
Assessment Answering Strategies
When responding to questions in a high-stakes evaluation, having a well-organized approach is key to success. The ability to interpret questions effectively and apply the right knowledge to each scenario is crucial for selecting the best possible responses. With a strategic approach, you can minimize errors and ensure that your answers reflect a solid understanding of critical concepts and procedures.
Key Approaches to Answering Effectively
To navigate through the evaluation process with confidence, consider the following strategies:
- Read Each Question Thoroughly – Take time to understand what is being asked before rushing to answer. Pay attention to keywords that highlight the core concepts of the question.
- Eliminate Clearly Incorrect Options – If the evaluation includes multiple-choice questions, rule out options that are obviously incorrect. This increases the likelihood of selecting the right answer from the remaining choices.
- Apply Knowledge of Protocols – Focus on the steps and best practices outlined in standard guidelines. Many questions are designed to assess your understanding of established protocols in emergency medical situations.
- Don’t Overthink – Trust your initial judgment when selecting answers. Often, the simplest and most straightforward answer is the correct one.
Improving Decision-Making Speed
In a time-sensitive evaluation, the ability to make quick, accurate decisions is essential. To improve your decision-making speed:
- Practice Frequently – Regularly review key concepts and test your knowledge through practice questions. The more familiar you are with the material, the faster you will be able to recall important details under pressure.
- Prioritize Critical Scenarios – Focus on questions that test your understanding of life-threatening situations. These are often weighted more heavily and require immediate recall of essential procedures.
By following these strategies, you can approach the evaluation process with greater confidence, ensuring that your answers reflect a well-rounded understanding of essential concepts and procedures in emergency care.
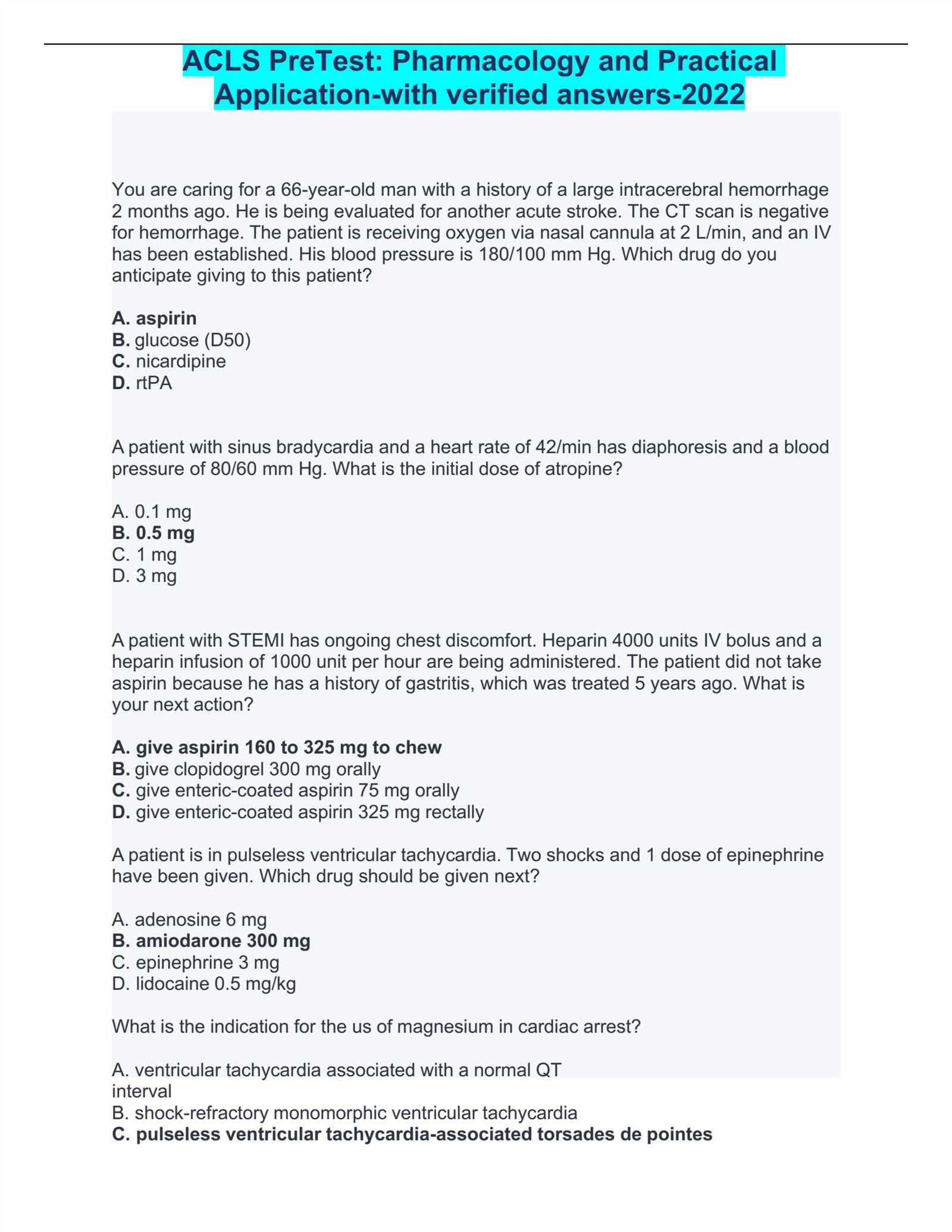
Reviewing Pharmacology Basics
In emergency medical care, understanding the pharmacological agents used in critical situations is essential for providing effective treatment. Medications play a pivotal role in stabilizing patients and managing life-threatening conditions such as cardiac arrest, arrhythmias, and respiratory distress. A solid foundation in pharmacology allows healthcare providers to make informed decisions about drug administration and ensure the best possible outcomes for their patients.
Key Drugs and Their Functions
Several medications are commonly used in emergency situations to treat a range of conditions. Below are some of the most frequently used drugs and their primary actions:
- Adrenaline (Epinephrine) – Used to stimulate the heart in cases of cardiac arrest, helping to improve circulation and increase the chances of a successful resuscitation.
- Amiodarone – A potent antiarrhythmic medication used to treat ventricular arrhythmias, including ventricular tachycardia and ventricular fibrillation.
- Lidocaine – Another antiarrhythmic used to treat abnormal heart rhythms, particularly during the early stages of a cardiac arrest scenario.
- Adenosine – Used to treat supraventricular tachycardia by slowing down the electrical conduction in the heart and restoring a normal rhythm.
- Atropine – Used in cases of bradycardia (slow heart rate) to increase the heart rate by blocking vagal stimulation.
Pharmacological Considerations in Critical Care
When administering medications in an emergency setting, it is important to consider factors such as the patient’s condition, the timing of drug administration, and potential side effects. Proper dosing, understanding contraindications, and being aware of drug interactions are critical components of safe and effective treatment. Additionally, recognizing the signs of toxicity or adverse reactions allows healthcare providers to make adjustments to the treatment plan as necessary.
- Proper Dosage – Adhering to recommended dosages ensures that drugs are effective without causing harm or unnecessary side effects.
- Timing – The timing of drug administration can significantly impact outcomes. Some medications, like adrenaline, should be administered as soon as possible, while others may be used at specific points in the resuscitation process.
- Monitoring – Continuous monitoring of the patient’s vital signs and response to medications is crucial for adjusting treatment as needed.
Having a comprehensive understanding of pharmacology basics is fundamental for making quick, accurate decisions in critical care settings. By being familiar with the drugs commonly used during emergencies, healthcare providers can confidently administer the appropriate treatment, improving patient outcomes and enhancing the quality of care provided.
Understanding Defibrillation and Its Use
Defibrillation is a critical medical procedure used to restore a normal heart rhythm in cases of severe cardiac arrhythmias, such as ventricular fibrillation and pulseless ventricular tachycardia. It involves delivering a controlled electric shock to the heart, which interrupts the chaotic electrical activity and allows the heart’s natural pacemaker to regain control. This intervention is essential for patients experiencing life-threatening irregularities in heart rhythm, and its timely application can significantly improve survival chances.
When Is Defibrillation Needed?
Defibrillation is typically required in emergency situations where a person’s heart is unable to pump blood effectively due to erratic electrical activity. Below are conditions where defibrillation is commonly indicated:
- Ventricular Fibrillation (VF) – A condition where the heart’s electrical activity becomes disorganized, causing the heart to quiver instead of contracting normally.
- Pulseless Ventricular Tachycardia (VT) – A fast, abnormal rhythm that prevents the heart from effectively pumping blood to the body.
- Sudden Cardiac Arrest (SCA) – A medical emergency where the heart suddenly stops beating due to an abnormal rhythm.
Types of Defibrillators and Their Use
There are several types of devices used for defibrillation, each with specific applications depending on the clinical scenario:
- Automated External Defibrillators (AEDs) – Portable devices that analyze the heart’s rhythm and automatically deliver a shock if needed. These are commonly found in public spaces and can be used by non-medical personnel with minimal training.
- Manual Defibrillators – Typically used by trained medical professionals, these devices require the operator to manually assess the heart rhythm and decide the appropriate shock energy and timing.
- Implantable Cardioverter Defibrillators (ICDs) – Small devices implanted in the chest that continuously monitor the heart’s rhythm and deliver shocks automatically when abnormal rhythms are detected.
Key Considerations During Defibrillation
For defibrillation to be effective, several important factors need to be considered:
- Timing – Defibrillation must be performed as soon as possible after the onset of a life-threatening arrhythmia. Delaying the shock can reduce the chances of survival.
- Shock Energy – The correct energy level should be selected based on the device and the condition being treated. Too low of a shock can be ineffective, while too high can cause further damage to the heart.
- Chest Compression Quality – Chest compressions should continue during the process to maintain blood flow to vital organs until the shock is delivered.
In emergency care, defibrillation plays a crucial role in saving lives. Understanding its use and ensuring timely intervention can make a significant difference in a patient’s outcome. Proper training and familiarity with the equipment are essential for healthcare providers to effectively use defibrillators in critical situations.
Managing Post-Cardiac Arrest Care
After a patient has been successfully resuscitated following a cardiac arrest, the next crucial phase of treatment involves managing post-resuscitation care. This period is vital for improving patient outcomes, preventing further complications, and ensuring adequate recovery. The care approach focuses on stabilizing the patient’s condition, optimizing organ function, and addressing any underlying causes that may have led to the arrest. Medical teams must work quickly and efficiently to provide comprehensive care during this critical period.
Key Components of Post-Resuscitation Care
Several factors must be carefully monitored and managed during the post-resuscitation phase:
- Hemodynamic Stabilization – Ensuring stable blood pressure and adequate circulation is essential to support organ function and prevent shock.
- Temperature Management – Therapeutic hypothermia (cooling) is often used to protect the brain and other vital organs from further injury after circulation has been restored.
- Ventilation and Oxygenation – Ensuring proper ventilation and oxygen levels is crucial to maintain adequate blood oxygen saturation and prevent respiratory complications.
Monitoring and Assessing Organ Function
Continual assessment of organ function is necessary to identify potential complications and provide timely interventions:
- Neurological Monitoring – Assessing brain function through neurological exams and imaging helps determine the extent of any damage sustained during the arrest and guides further care decisions.
- Cardiac Function – Monitoring heart rhythm and function is critical to detect arrhythmias or other cardiovascular issues that may arise post-arrest.
- Renal and Liver Function – Kidney and liver function should be assessed as they can be impacted by reduced blood flow during the arrest.
Managing post-resuscitation care effectively requires a multidisciplinary approach, involving careful monitoring, prompt intervention, and ongoing support for the patient. By addressing these key areas, healthcare teams can improve the chances of recovery and reduce the risks of complications that may arise after a cardiac arrest event.
Preparing for the Skills Test
When preparing for an advanced life support skills examination, it is essential to focus on mastering the practical components required to manage emergencies effectively. The test evaluates a healthcare provider’s ability to respond to various critical situations, including managing airway obstructions, cardiac arrests, and severe arrhythmias. A solid understanding of the techniques involved, along with practice, is key to performing confidently and competently under pressure.
Focus on Key Skills
Several critical skills need to be practiced and refined before taking the skills test. These skills typically include:
- Airway Management – Learning to effectively secure an airway using various devices and techniques is crucial for ensuring proper oxygenation and ventilation during emergencies.
- CPR and Chest Compressions – High-quality chest compressions are vital for maintaining circulation during cardiac arrest. Proper technique and timing are essential for effective resuscitation.
- Defibrillation – Knowing how and when to use an automated external defibrillator (AED) to restore a normal rhythm in a patient with arrhythmia is a critical skill.
Simulation and Practice
Practicing with realistic simulations can help familiarize individuals with high-stress situations and improve their response time. Key actions to focus on during practice include:
- Teamwork – Efficient communication and coordination with fellow team members are vital for providing optimal care during a resuscitation attempt.
- Decision-Making – Rapid, accurate decisions are necessary to adjust care protocols based on the patient’s response and the evolving situation.
Preparing thoroughly for the skills exam ensures not only a successful test outcome but also builds the confidence and competence needed to provide critical care in real-life scenarios.
Guidelines for Effective Team Communication
In high-pressure situations, such as medical emergencies, effective communication within a team is critical for delivering rapid and coordinated care. Clear, concise, and timely communication ensures that each team member understands their role and actions, leading to better patient outcomes. When performing resuscitation or handling a life-threatening scenario, miscommunication can lead to delays, mistakes, or confusion, making it essential to establish clear communication protocols ahead of time.
Key Communication Strategies
To enhance communication during emergencies, the following guidelines can help facilitate smooth interaction among team members:
- Clear and Concise Instructions – Speak in short, direct phrases. Avoid jargon or unnecessary details to ensure that everyone can quickly grasp the message and respond appropriately.
- Use of Closed-Loop Communication – Acknowledge and repeat back instructions to confirm understanding. For example, if a team member directs a task, the listener should repeat the instruction before proceeding.
- Maintain Calm and Focus – In stressful situations, staying composed and focused on the task at hand is essential. Clear communication becomes even more critical when emotions run high.
- Non-Verbal Cues – In noisy or chaotic environments, non-verbal signals such as hand gestures, eye contact, or nodding can convey vital information without the need for verbal communication.
Role Clarity and Leadership
Every member of the team should have a defined role, and a clear leader should be identified to direct actions. These roles may include:
- Leader – Oversees the overall management of the situation and provides guidance to other team members.
- Airway Manager – Focuses on maintaining or securing the patient’s airway, ensuring proper ventilation and oxygenation.
- Chest Compressor – Responsible for performing high-quality chest compressions during resuscitation.
- Defibrillator Operator – Manages the use of defibrillation equipment when necessary to restore a normal rhythm.
By following these communication strategies and clearly defining team roles, medical teams can work together more efficiently, ultimately improving the chances of a positive outcome in critical situations.
Algorithms You Should Know
In emergency situations, particularly those involving life-threatening cardiac events, following well-established procedures is essential to ensure the best chance of survival. These procedures, commonly referred to as algorithms, provide a step-by-step guide for healthcare professionals to follow when managing critical situations. Understanding and memorizing these algorithms is crucial for delivering timely and effective care.
The following table highlights some of the key algorithms that every medical professional should be familiar with when responding to cardiac emergencies. These algorithms outline essential steps for different scenarios and help guide treatment decisions quickly and efficiently.
| Algorithm | Description | Key Actions |
|---|---|---|
| Cardiac Arrest | Steps for managing a patient who has no pulse and is not breathing | Initiate CPR, assess rhythm, deliver shocks if indicated, continue resuscitation efforts |
| Bradycardia | Management of slow heart rates that cause symptoms | Administer atropine, consider transcutaneous pacing if symptoms persist |
| Tachycardia with Pulse | Approach for managing patients with a rapid heart rate and a pulse | Identify the rhythm, consider synchronized cardioversion, administer antiarrhythmic medications |
| Acute Coronary Syndrome | Steps for managing a patient suspected of having a heart attack | Administer aspirin, nitroglycerin, and morphine as appropriate, monitor EKG |
| Stroke | Procedure for evaluating and treating patients with signs of a stroke | Perform rapid neurological assessment, consider thrombolytics if within the therapeutic window |
Familiarity with these algorithms ensures that medical professionals can act decisively in critical moments, optimizing patient care and improving survival rates. Regular practice and ongoing training are essential to staying proficient in these life-saving procedures.
How the Assessment Helps Your Certification
Completing a preliminary evaluation before taking the practical skills test plays a crucial role in preparing individuals for their certification. This evaluation serves as both a self-assessment and a guide to the core concepts that will be tested. It helps identify areas of strength and weaknesses, allowing participants to focus on critical topics before the official certification process. By ensuring a solid understanding of the material, the evaluation contributes directly to the successful completion of the certification.
Identifying Knowledge Gaps
The evaluation process helps pinpoint any gaps in knowledge, ensuring that all essential areas are covered. When individuals can clearly identify areas where their understanding is lacking, they are able to target those topics for further review, increasing the chances of mastering the material before the certification exam.
Boosting Confidence
By engaging in a self-assessment, individuals can become more familiar with the types of questions and topics they will encounter. This not only builds confidence but also reduces the anxiety associated with taking the certification exam. Knowing what to expect and recognizing one’s own preparedness can lead to better performance when it matters most.
Ultimately, this preliminary step serves as a critical foundation for success in the certification process. It ensures that individuals are well-prepared, informed, and capable of meeting the challenges of the exam, significantly increasing their likelihood of certification achievement.
Resources for Pre Course Preparation
Effective preparation for the certification process requires access to a variety of educational materials. These resources can help individuals familiarize themselves with the key concepts, terminology, and procedures they will need to understand. By utilizing different types of content, learners can enhance their knowledge and increase their confidence before the actual exam.
Recommended Learning Materials
There are several types of materials available to assist with the preparation process, each offering unique benefits:
- Online Tutorials: Interactive platforms provide engaging lessons that cover essential topics and test your understanding through quizzes and videos.
- Textbooks and Manuals: Comprehensive written resources offer in-depth explanations of key concepts and guidelines, often including case studies and practical scenarios.
- Practice Exams: Timed quizzes and sample tests simulate the exam environment, helping you become familiar with the format and manage time effectively during the real test.
- Instructional Videos: Visual demonstrations of key procedures and techniques can improve your understanding of complex tasks and techniques.
- Workshops and Training Sessions: In-person or virtual workshops allow participants to practice skills under the supervision of experienced professionals, providing immediate feedback.
Additional Tools and Support
Along with traditional resources, there are also several tools and support systems available to help individuals during their preparation:
- Study Groups: Connecting with others who are preparing for the same certification can offer valuable insights, allow for the exchange of study tips, and foster a sense of camaraderie.
- Mobile Apps: Many apps provide easy-to-use resources for on-the-go learning, such as flashcards, quizzes, and key concept reviews.
- Forums and Online Communities: Online forums provide a platform for discussing questions, sharing experiences, and seeking advice from those who have already completed the process.
By leveraging these diverse learning resources, individuals can approach the certification process with a comprehensive understanding and well-prepared mindset, increasing their likelihood of success.