Normal Ear Exam Documentation for Accurate Diagnosis
In the healthcare field, a detailed examination of the auditory system is essential for identifying potential issues and ensuring overall well-being. Proper recording of findings during this process plays a crucial role in making informed decisions about treatment and care. It is not only about identifying symptoms but also about accurately capturing the condition for future reference and communication with other professionals.
Accurate and thorough documentation helps create a clear understanding of the patient’s condition. By carefully noting observations and measurements, healthcare providers ensure that nothing is overlooked and that all information is available for follow-up appointments or further investigations. This structured approach enhances both the quality and consistency of care.
Efficient record-keeping is vital for providing a comprehensive view of a patient’s health. The ability to track changes over time and compare findings ensures that appropriate steps are taken to address any underlying issues. This section will explore the essential aspects of a systematic approach to assessment and the role of well-documented health records in facilitating effective patient management.
Comprehensive Assessment Recording
Accurate recording of health checks for the auditory system is a vital part of patient care. By systematically documenting findings, healthcare professionals can ensure that critical information is preserved for future reference. This process not only helps identify potential issues but also supports ongoing monitoring and effective treatment planning.
Essential Elements of Record-Keeping
Effective note-taking involves capturing a range of details observed during the assessment. This includes noting the patient’s medical history, any discomfort or symptoms reported, and visual or physical findings. A clear and organized record enables healthcare providers to quickly access relevant information, aiding in diagnosis and treatment decisions.
Best Practices for Accurate Notation
Consistency is key to ensuring that records are reliable and useful. Using standardized forms or templates can help maintain uniformity across assessments, making it easier to compare results over time. Thoroughness in documenting observations ensures no important detail is missed, ultimately contributing to a more comprehensive understanding of the patient’s health status.
Comprehensive Assessment Recording
Accurate recording of health checks for the auditory system is a vital part of patient care. By systematically documenting findings, healthcare professionals can ensure that critical information is preserved for future reference. This process not only helps identify potential issues but also supports ongoing monitoring and effective treatment planning.
Essential Elements of Record-Keeping
Effective note-taking involves capturing a range of details observed during the assessment. This includes noting the patient’s medical history, any discomfort or symptoms reported, and visual or physical findings. A clear and organized record enables healthcare providers to quickly access relevant information, aiding in diagnosis and treatment decisions.
Best Practices for Accurate Notation
Consistency is key to ensuring that records are reliable and useful. Using standardized forms or templates can help maintain uniformity across assessments, making it easier to compare results over time. Thoroughness in documenting observations ensures no important detail is missed, ultimately contributing to a more comprehensive understanding of the patient’s health status.
Key Components of Auditory Health Assessment
Assessing the health of the auditory system involves several essential elements that help in identifying potential concerns and ensuring overall well-being. Each component plays a crucial role in creating a comprehensive picture of the patient’s condition. From gathering relevant history to performing specific tests, each step helps to highlight any issues that may require attention.
The first step in a thorough evaluation is understanding the patient’s medical history, as it can provide valuable context for interpreting symptoms and signs. Following that, physical observations, such as inspecting the outer structures and assessing any visible abnormalities, are critical. Additionally, functional tests are conducted to measure the efficiency of the auditory mechanisms and identify potential areas of concern.
Incorporating a structured approach ensures that no aspect of the assessment is overlooked, and it enables healthcare providers to make informed decisions regarding treatment or further investigation. Accurate documentation of each element is also essential for tracking the patient’s condition over time and ensuring continuity of care.
Step-by-Step Auditory Inspection Procedure
Performing a thorough inspection of the auditory system requires a systematic approach to ensure that no detail is overlooked. Each step serves a specific purpose, from initial observation to more detailed analysis. Following a structured procedure allows for consistent and accurate results, which are essential for identifying any underlying issues and guiding appropriate treatment.
Begin with the patient’s medical history, gathering information on previous conditions, symptoms, or family history that may provide context for the current examination. Next, conduct a visual inspection of the outer structures, looking for signs of injury, swelling, or other abnormalities. A careful examination of the surrounding areas, including the scalp and neck, is also important for identifying any issues that may impact the auditory system.
Once the external inspection is complete, move on to more detailed procedures such as testing the response to sounds or checking for physical blockages. Each step should be documented clearly to ensure accuracy and provide a comprehensive record for future reference. By following this methodical approach, healthcare providers can ensure that all potential issues are addressed and that the patient’s auditory health is well understood.
Documenting Auditory Canal Observations
When assessing the auditory canal, it is important to carefully record any visual findings that may indicate abnormalities or potential issues. Clear and accurate notes ensure that no critical information is overlooked and help in tracking any changes over time. A structured approach to documenting these observations can provide valuable insights into a patient’s auditory health.
Key Observations to Record
- Condition of the Canal: Note any signs of redness, swelling, or injury.
- Presence of Obstructions: Record if there is any buildup of wax or foreign objects.
- Discharge: Document the color, consistency, and quantity of any fluid present.
- Temperature: Check for signs of infection, such as warmth or tenderness.
- Structural Irregularities: Observe any deformities, scarring, or abnormalities in the canal shape.
Each of these factors should be carefully noted to provide a comprehensive view of the patient’s condition. Proper documentation allows healthcare providers to make informed decisions, ensuring the best possible care. Regular updates to the record are important, especially if there are any changes or developments in the patient’s symptoms or condition.
Identifying Common Auditory System Conditions
Recognizing common conditions affecting the auditory system is essential for providing timely and appropriate care. By identifying the key signs and symptoms associated with these conditions, healthcare providers can ensure effective treatment and management. Properly documenting these findings allows for accurate tracking and comparison over time, which is crucial for diagnosing and monitoring progress.
Common Conditions to Watch For
- Infections: Look for signs of redness, discharge, or swelling that may indicate an infection, such as otitis media or external ear infections.
- Blockages: Cerumen buildup or foreign objects in the canal can cause discomfort and hearing loss. Always check for obstructions.
- Tinnitus: Document patient reports of ringing or buzzing sounds, which could point to underlying issues like noise-induced hearing loss or inner ear problems.
- Trauma: Any visible injury to the external structures, such as cuts or bruising, should be noted as it could affect hearing or lead to further complications.
Signs of More Serious Conditions
- Sudden Hearing Loss: Sudden or unexplained hearing loss should be documented and assessed immediately as it can indicate serious conditions like a ruptured eardrum or vestibular disorder.
- Fluid Discharge: Unusual discharge, especially if it’s persistent or accompanied by pain, may suggest an infection or injury that requires immediate attention.
Accurate identification and documentation of these common conditions are critical for providing effective patient care. By noting these symptoms and any changes, healthcare professionals can make informed decisions and offer the best treatment options available.
Recording Tympanic Membrane Findings
Accurate recording of tympanic membrane (eardrum) findings is crucial in evaluating auditory health. Observing the condition of this membrane helps in diagnosing potential infections, trauma, or other conditions that may affect hearing. Thorough documentation ensures that these important observations are preserved for future reference, aiding in treatment decisions and long-term care.
| Observation | Possible Condition |
|---|---|
| Color: Pink or light gray | Healthy membrane |
| Redness or inflammation: Dark red or swollen | Infection (e.g., otitis media) |
| Perforation: Hole or tear | Tympanic membrane rupture or trauma |
| Fluid: Visible fluid behind membrane | Middle ear infection or effusion |
| Bulging: Swelling outward | Pressure buildup due to infection or fluid |
When documenting these observations, it is important to be specific and consistent. Each detail, from the appearance to any signs of abnormality, should be clearly noted. This allows healthcare providers to track any changes over time, ensuring timely and effective management of any identified issues.
Importance of Patient History in Auditory Assessments

Understanding a patient’s medical background is a critical component of any thorough evaluation of auditory health. A detailed history provides essential context that helps healthcare providers interpret current symptoms, identify risk factors, and make more accurate diagnoses. Gathering this information can significantly improve the effectiveness of subsequent procedures and contribute to more personalized care.
The patient’s history can reveal prior conditions, previous treatments, or family history of hearing-related issues, which may indicate an increased risk of certain conditions. Additionally, any recent symptoms, such as pain, discomfort, or changes in hearing, should be documented to help guide the assessment process. This information not only aids in identifying underlying causes but also helps in monitoring the patient’s progress over time.
By carefully considering the patient’s history, healthcare providers can make better-informed decisions, select appropriate diagnostic tests, and develop targeted treatment plans. Comprehensive documentation of this history is crucial for continuity of care and for future reference in case of any changes or recurring issues.
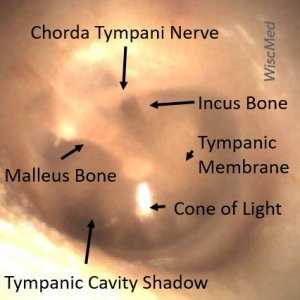
Using Otoscope for Detailed Auditory System Examination
The otoscope is a vital tool for performing a comprehensive inspection of the auditory system. By providing a clear, magnified view of the canal and surrounding structures, it allows healthcare providers to identify potential issues that may not be visible to the naked eye. The device aids in detecting abnormalities such as infections, blockages, or injuries that could affect hearing and overall health.
Steps for Using the Otoscope Effectively
- Preparation: Ensure the otoscope is properly sanitized and the appropriate size speculum is selected for the patient’s comfort.
- Positioning: Gently hold the otoscope while positioning the speculum at the opening of the auditory canal.
- Inspection: Slowly insert the speculum into the canal, observing the structures and noting any irregularities such as redness, swelling, or blockages.
- Documentation: Record the findings, including the appearance of the canal, any obstructions, or signs of infection, to provide a clear account of the examination.
Key Areas to Examine with the Otoscope
- Canal Condition: Look for any abnormal color, swelling, or signs of injury.
- Presence of Fluid or Blockages: Check for any obstructions such as earwax buildup or foreign objects.
- Tympanic Membrane: Observe the appearance of the membrane, checking for signs of perforation, fluid, or inflammation.
By using the otoscope correctly and following these steps, healthcare providers can ensure a thorough evaluation of the auditory system, which is essential for accurate diagnosis and treatment.
Assessing Auditory Discomfort and Pain
Identifying and evaluating discomfort or pain in the auditory region is crucial for diagnosing underlying issues. These sensations can stem from a range of causes, from infections to blockages or trauma. Proper assessment of the patient’s symptoms, along with a detailed history, helps determine the root cause and guide appropriate treatment strategies.
Identifying Pain Characteristics
- Location: Determine whether the pain is localized to a specific area or radiates to other parts of the head or neck.
- Duration: Assess how long the pain has been present, whether it is constant or intermittent, and if there are any patterns or triggers.
- Intensity: Ask the patient to rate the severity of the pain on a scale from mild to severe.
Possible Causes of Discomfort
- Infections: Inflammation or infection in the auditory canal or middle regions often results in pain and tenderness.
- Blockages: A buildup of earwax or foreign objects can cause pressure and discomfort.
- Trauma: Injury or excessive pressure, such as from sudden changes in altitude, can lead to sharp pain or a feeling of fullness.
- Pressure Changes: Changes in atmospheric pressure, such as while flying, can cause discomfort or a sensation of blockage.
Accurate evaluation of these symptoms is vital for determining whether the cause is minor or requires more immediate medical intervention. Clear documentation of pain details, combined with other findings, will guide treatment decisions and help ensure effective care.
Assessing Auditory Discomfort and Pain
Identifying and evaluating discomfort or pain in the auditory region is crucial for diagnosing underlying issues. These sensations can stem from a range of causes, from infections to blockages or trauma. Proper assessment of the patient’s symptoms, along with a detailed history, helps determine the root cause and guide appropriate treatment strategies.
Identifying Pain Characteristics
- Location: Determine whether the pain is localized to a specific area or radiates to other parts of the head or neck.
- Duration: Assess how long the pain has been present, whether it is constant or intermittent, and if there are any patterns or triggers.
- Intensity: Ask the patient to rate the severity of the pain on a scale from mild to severe.
Possible Causes of Discomfort
- Infections: Inflammation or infection in the auditory canal or middle regions often results in pain and tenderness.
- Blockages: A buildup of earwax or foreign objects can cause pressure and discomfort.
- Trauma: Injury or excessive pressure, such as from sudden changes in altitude, can lead to sharp pain or a feeling of fullness.
- Pressure Changes: Changes in atmospheric pressure, such as while flying, can cause discomfort or a sensation of blockage.
Accurate evaluation of these symptoms is vital for determining whether the cause is minor or requires more immediate medical intervention. Clear documentation of pain details, combined with other findings, will guide treatment decisions and help ensure effective care.
How to Document Auditory Discharge
When assessing any fluid coming from the auditory region, it is important to record the key characteristics for accurate diagnosis and effective treatment. Properly noting these observations helps healthcare providers identify potential infections, blockages, or other conditions that may require intervention. Accurate documentation ensures ongoing monitoring and informs future treatment decisions.
Essential Characteristics to Record
- Color: Identify the color of the discharge, such as clear, yellow, green, or blood-tinged.
- Consistency: Record whether the discharge is watery, thick, or purulent.
- Amount: Note whether the discharge is minimal, moderate, or excessive.
- Odor: Indicate if there is any foul or unusual smell, which could suggest an infection.
Table for Fluid Discharge Documentation
| Characteristic | Details |
|---|---|
| Color | Clear, Yellow, Green, Bloody, etc. |
| Consistency | Watery, Thick, Purulent, etc. |
| Amount | Minimal, Moderate, Excessive |
| Odor | Foul, None, Unusual |
By documenting these factors, healthcare providers can assess the nature and possible causes of the discharge, enabling them to offer the most appropriate treatment. This process is crucial for tracking the progression of conditions and ensuring comprehensive care for the patient.
Effective Use of Auditory Assessment Templates
Utilizing structured templates for auditory evaluations streamlines the process of recording observations, ensuring consistency and accuracy. These tools help healthcare providers efficiently document key findings, which is essential for tracking patient progress and ensuring proper care. A well-designed template can enhance the quality of assessments, reduce errors, and save time during patient evaluations.
Benefits of Using Templates
- Consistency: Templates provide a standardized format, ensuring all critical areas are consistently documented for every patient.
- Efficiency: By pre-filling common sections, templates reduce the time spent on repetitive tasks, allowing more focus on patient interaction.
- Accuracy: Templates guide the examiner through key areas, minimizing the chance of overlooking important details or findings.
- Better Communication: Structured templates help communicate findings clearly across the healthcare team, aiding in collaborative decision-making.
Key Sections to Include in Templates
- Patient History: Basic information about the patient’s medical background, previous conditions, or concerns that may affect the assessment.
- Symptom Description: Space to document the patient’s complaints, such as discomfort, pain, or hearing issues.
- Physical Findings: Sections for documenting visual observations, such as the condition of the auditory canal and tympanic membrane.
- Diagnostic Tests: If applicable, a section for recording results from additional diagnostic procedures, such as hearing tests or imaging.
- Treatment Plan: An area for outlining the recommended treatment or follow-up procedures based on the assessment.
By incorporating these key elements, templates ensure that the assessment process is thorough, organized, and easily accessible for future reference. Proper use of templates not only improves clinical workflow but also enhances patient care through more accurate and timely assessments.
Best Practices for Accurate Record-Keeping
Maintaining precise and reliable records is essential in any healthcare setting. It ensures that patient information is documented consistently, enabling healthcare providers to make informed decisions and track progress effectively. Adopting best practices in recording assessments not only reduces errors but also improves the overall quality of care provided.
Key Guidelines for Effective Record-Keeping
- Clarity and Precision: Always be clear and specific when documenting findings. Avoid ambiguous terms that could lead to misinterpretation, and ensure that descriptions are detailed yet concise.
- Consistency: Use standardized language and formats across all patient records. This includes consistent terminology and measurement units, making it easier to compare different assessments.
- Timeliness: Record observations as soon as possible after the assessment. Immediate documentation reduces the risk of forgetting important details and ensures that the information remains accurate.
- Objectivity: Focus on facts and avoid subjective opinions. Document only what was observed, heard, or tested, and refrain from including personal interpretations or assumptions.
- Comprehensive Coverage: Ensure all relevant information is documented, including patient complaints, physical findings, and any additional tests or procedures performed. Don’t leave out critical details that could affect diagnosis or treatment.
Ensuring Accuracy in Patient Records
- Use Structured Templates: Templates help standardize the process and ensure that no important data is omitted. Pre-filled sections can also make the documentation process more efficient.
- Verify Information: Double-check details, especially if any data was obtained from other sources or patients themselves. This helps avoid mistakes and enhances reliability.
- Maintain Confidentiality: Always ensure that records are kept secure and that patient privacy is respected, following the appropriate legal and ethical guidelines.
By implementing these best practices, healthcare professionals can maintain a high standard of accuracy and efficiency in record-keeping, ultimately contributing to better patient care and smoother clinical workflows.
Legal Considerations in Assessment Reports
In healthcare, proper documentation is not only vital for clinical purposes but also carries significant legal implications. Accurate and thorough records ensure that healthcare professionals can defend their actions in case of disputes or legal proceedings. Understanding the legal aspects of record-keeping is essential for protecting both the patient and the provider.
Key Legal Principles to Consider
- Confidentiality and Privacy: All patient-related information must be kept confidential in accordance with healthcare privacy laws such as HIPAA (Health Insurance Portability and Accountability Act) in the United States or similar regulations in other countries. Unauthorized access or disclosure of patient records can lead to severe legal consequences.
- Accuracy and Completeness: Inaccurate or incomplete documentation can undermine the legal value of the report. It is critical that every entry is clear, objective, and thoroughly reflects the findings. Any omissions could potentially be viewed as negligence in a legal context.
- Timeliness of Documentation: Timely recording of patient assessments and findings is essential. Delay in documentation may be interpreted as a failure to provide appropriate care or as an attempt to falsify records in the event of a claim or lawsuit.
- Signatures and Authentication: All documentation must be properly signed, dated, and authenticated. This includes confirming that the healthcare professional who conducted the assessment is the one who recorded the findings, ensuring accountability and traceability of the data.
- Clear Distinction Between Fact and Opinion: When documenting findings, it is essential to differentiate between observed facts and subjective opinions. Misrepresenting facts or making unsupported conclusions can expose the provider to liability in the event of litigation.
Table: Common Legal Issues in Medical Record-Keeping
| Issue | Description | Legal Consequences |
|---|---|---|
| Inaccurate Documentation | Failure to accurately record patient findings can lead to misunderstandings and affect the care provided. | Potential malpractice claims and loss of credibility in court. |
| Unauthorized Access | Failure to protect patient records or sharing information without consent violates privacy laws. | Legal action under privacy laws, fines, and loss of professional license. |
| Delays in Record-Keeping | Delayed documentation may suggest negligence or attempt to alter records. | Damaged legal defense, potential malpractice claims. |
By adhering to these legal considerations, healthcare providers can mitigate risk and ensure their records are reliable and defensible in case of legal scrutiny.
Common Mistakes in Health Assessment Reports
Accurate and thorough record-keeping is critical in healthcare, yet many providers make errors that can compromise the quality of care and even lead to legal or clinical issues. Understanding the most common mistakes made during patient evaluations and taking steps to avoid them can ensure better patient outcomes and protect healthcare providers from potential liability.
Common Errors in Patient Record-Keeping
- Omissions in Key Findings: Failing to document important observations or details can result in incomplete records. This could lead to misunderstandings regarding the patient’s condition and care plan, potentially compromising treatment decisions.
- Vague or Unclear Language: Using unclear or ambiguous terms to describe symptoms or findings can cause confusion. Documentation should be precise and specific to ensure the information is easily understood by other healthcare providers.
- Inaccurate or Misleading Information: Providing incorrect data or interpreting findings incorrectly is a serious mistake. Misleading documentation could lead to improper treatment or even legal claims.
- Failure to Include Patient History: Patient history is an essential part of any assessment. Failing to document past conditions, treatments, or family history may hinder the ability to make informed clinical decisions.
- Not Timely Documenting Findings: Delays in documentation can lead to inaccuracies or omissions. It’s important to record findings as soon as possible to avoid forgetting key details or making retrospective errors.
Table: Common Mistakes in Health Assessment and Their Impact
| Mistake | Potential Impact | How to Avoid |
|---|---|---|
| Omissions in Key Findings | Incomplete or incorrect treatment decisions. | Ensure all significant symptoms and findings are documented clearly. |
| Vague or Unclear Language | Confusion among healthcare providers and risk of misinterpretation. | Use precise terminology and avoid medical jargon when possible. |
| Inaccurate or Misleading Information | Incorrect treatment or medication, leading to poor patient outcomes. | Double-check facts and ensure all observations are supported by evidence. |
| Failure to Include Patient History | Failure to recognize underlying conditions, leading to inappropriate care. | Document all relevant patient history in every report. |
| Not Timely Documenting Findings | Loss of important details or retrospective errors. | Document findings immediately after assessment to avoid errors. |
By being aware of these common pitfalls and taking proactive steps to avoid them, healthcare providers can maintain high standards of patient care and ensure that records are both accurate and effective for clinical decision-making.
Common Mistakes in Health Assessment Reports
Accurate and thorough record-keeping is critical in healthcare, yet many providers make errors that can compromise the quality of care and even lead to legal or clinical issues. Understanding the most common mistakes made during patient evaluations and taking steps to avoid them can ensure better patient outcomes and protect healthcare providers from potential liability.
Common Errors in Patient Record-Keeping
- Omissions in Key Findings: Failing to document important observations or details can result in incomplete records. This could lead to misunderstandings regarding the patient’s condition and care plan, potentially compromising treatment decisions.
- Vague or Unclear Language: Using unclear or ambiguous terms to describe symptoms or findings can cause confusion. Documentation should be precise and specific to ensure the information is easily understood by other healthcare providers.
- Inaccurate or Misleading Information: Providing incorrect data or interpreting findings incorrectly is a serious mistake. Misleading documentation could lead to improper treatment or even legal claims.
- Failure to Include Patient History: Patient history is an essential part of any assessment. Failing to document past conditions, treatments, or family history may hinder the ability to make informed clinical decisions.
- Not Timely Documenting Findings: Delays in documentation can lead to inaccuracies or omissions. It’s important to record findings as soon as possible to avoid forgetting key details or making retrospective errors.
Table: Common Mistakes in Health Assessment and Their Impact
| Mistake | Potential Impact | How to Avoid |
|---|---|---|
| Omissions in Key Findings | Incomplete or incorrect treatment decisions. | Ensure all significant symptoms and findings are documented clearly. |
| Vague or Unclear Language | Confusion among healthcare providers and risk of misinterpretation. | Use precise terminology and avoid medical jargon when possible. |
| Inaccurate or Misleading Information | Incorrect treatment or medication, leading to poor patient outcomes. | Double-check facts and ensure all observations are supported by evidence. |
| Failure to Include Patient History | Failure to recognize underlying conditions, leading to inappropriate care. | Document all relevant patient history in every report. |
| Not Timely Documenting Findings | Loss of important details or retrospective errors. | Document findings immediately after assessment to avoid errors. |
By being aware of these common pitfalls and taking proactive steps to avoid them, healthcare providers can maintain high standards of patient care and ensure that records are both accurate and effective for clinical decision-making.