Comprehensive Pelvic Exam Template for Healthcare Providers
Healthcare professionals rely on structured frameworks to ensure consistency and accuracy during medical evaluations. These frameworks help in conducting thorough examinations while maintaining a clear record of findings. Such systematic approaches are essential for diagnosing and monitoring various conditions related to reproductive health.
Standardized procedures play a crucial role in ensuring that each assessment is both comprehensive and effective. By following a well-organized structure, medical practitioners can identify potential concerns early and make informed decisions regarding treatment. This process is especially important for sensitive health evaluations, where patient comfort and trust are of paramount importance.
With a reliable method in place, healthcare providers can offer better care, increase patient confidence, and reduce the risk of missed diagnoses. The goal is to create a process that is efficient, easy to follow, and adaptable to different patient needs and circumstances.
Pelvic Exam Template Overview
In healthcare, having a structured approach for conducting thorough assessments is essential. A clear framework guides professionals through every step of the process, ensuring that no important detail is overlooked. This systematic method not only improves the accuracy of the evaluation but also promotes consistency across different providers and settings.
Effective documentation plays a key role in tracking patient health over time. By recording findings in a standardized manner, healthcare providers can monitor changes, diagnose issues earlier, and make better-informed decisions regarding treatment. Such frameworks also enhance communication among team members, ensuring that all relevant information is shared efficiently.
Additionally, a well-designed structure helps maintain a respectful and comfortable environment for patients. By following a consistent procedure, professionals can make the experience less stressful for individuals undergoing sensitive health evaluations. The overall goal is to create a process that is both thorough and compassionate, fostering trust between patient and provider.
Importance of Standardizing Pelvic Exams
Consistency in medical procedures is essential for providing high-quality care. Standardizing healthcare assessments ensures that all patients receive the same level of attention and thoroughness, regardless of the healthcare provider. A uniform approach reduces the risk of errors, enhances accuracy, and improves overall outcomes by adhering to established guidelines.
Improved Accuracy and Diagnosis
When healthcare professionals follow a structured procedure, they can more easily identify abnormalities or signs of potential issues. Standardization helps ensure that no critical detail is overlooked, leading to better diagnoses and more effective treatment plans. By using a consistent approach, the chances of missing key symptoms are minimized, which can be crucial for early intervention.
Patient Confidence and Comfort
Standardizing medical assessments also plays a significant role in enhancing patient trust. Knowing that their care is being provided in a consistent and systematic manner can help reduce anxiety, especially during sensitive procedures. A structured approach ensures that patients feel more comfortable, knowing that every step is designed with their well-being in mind.
Key Components of a Pelvic Exam
In any comprehensive health evaluation, there are essential elements that ensure a thorough assessment of a patient’s condition. These components help healthcare professionals gather critical information, identify potential concerns, and provide accurate diagnoses. By focusing on these key factors, the procedure can be conducted efficiently and with attention to detail.
Patient history and communication are fundamental starting points. A clear understanding of the patient’s medical background, symptoms, and concerns helps guide the assessment. Effective communication allows the healthcare provider to address any questions or discomfort the patient may experience during the process.
Physical examination is the core of the evaluation, where the healthcare professional visually inspects and palpates the relevant areas. This step provides crucial insights into any physical abnormalities or signs of illness that may require further investigation.
Lab tests and screenings are often incorporated into the assessment process to detect infections, abnormalities, or other health concerns. These tests add an important layer of diagnostic accuracy and ensure that any underlying issues are properly addressed.
Steps to Prepare for a Pelvic Exam
Proper preparation is essential to ensure that a health assessment is conducted smoothly and efficiently. Both the healthcare provider and the patient must be ready for the procedure, which includes gathering necessary information, setting up the environment, and making the patient feel as comfortable as possible.
Patient Education is one of the first steps. Ensuring that the patient understands the purpose of the assessment and what to expect can help reduce anxiety and increase cooperation. Clear explanations about the procedure, as well as answering any questions, can help set the tone for a more positive experience.
Creating a Comfortable Environment is key to helping the patient feel at ease. A private, clean, and warm setting can make a significant difference in the patient’s comfort level. Ensuring that the patient has adequate privacy and reassurance before the procedure can lead to better results and a smoother process.
Gathering Medical History before the assessment is also crucial. Reviewing the patient’s medical background, any symptoms they may have, and previous health concerns will help guide the procedure and inform the healthcare provider of any specific areas of focus.
How to Document Pelvic Exam Results
Accurate and detailed documentation is essential for tracking patient health and ensuring continuity of care. Properly recording the findings of any health assessment not only helps in diagnosis but also allows healthcare professionals to monitor changes over time. It is important that results are documented clearly, using standardized methods, to ensure that they can be easily interpreted by other healthcare providers.
When documenting results, it is essential to include both objective findings and the patient’s subjective reports. This provides a complete picture of the individual’s health status and any areas that may require further attention. Using a consistent format for each evaluation ensures clarity and makes it easier to compare results across different assessments.
| Category | Details |
|---|---|
| Visual Inspection | Note any abnormalities in appearance, such as swelling, discoloration, or lesions. |
| Palpation | Document tenderness, masses, or any unusual findings during palpation. |
| Patient Complaints | Include any concerns the patient reports, such as pain or discomfort in specific areas. |
| Tests and Screenings | Record any tests performed, along with their results, if applicable. |
| Follow-Up Recommendations | Document suggested next steps, including referrals, further testing, or treatment plans. |
By using a structured approach to record findings, healthcare providers can ensure that important information is not missed and that patients receive the best possible care.
Best Practices for Conducting Pelvic Exams
Following best practices during any health assessment ensures both the accuracy of the results and the comfort of the patient. These practices not only help in obtaining reliable data but also play a crucial role in establishing trust between healthcare providers and patients. A systematic approach is essential to guarantee that all relevant areas are thoroughly examined while maintaining the highest standards of patient care.
It is important to maintain a professional and respectful environment throughout the procedure. Proper patient communication, clear explanations of each step, and ensuring their comfort are fundamental to a positive experience. Additionally, a structured approach to performing the examination reduces the likelihood of overlooking important findings.
| Best Practice | Details |
|---|---|
| Prepare the Patient | Ensure the patient understands the procedure and feels comfortable with the process. |
| Maintain Privacy | Ensure the patient’s privacy and comfort, using drapes and proper positioning during the assessment. |
| Use Gentle Techniques | Be gentle and patient when conducting any physical assessments to minimize discomfort. |
| Record Findings Accurately | Document all observations clearly, including patient complaints, physical findings, and test results. |
| Provide Clear Instructions | Guide the patient through each step of the process to alleviate anxiety and confusion. |
By adhering to these best practices, healthcare providers can ensure that their assessments are both thorough and respectful, fostering a positive and effective healthcare experience.
Common Conditions Detected During Pelvic Exam
Routine health assessments can reveal a variety of conditions that may otherwise go unnoticed. Early detection through a thorough examination allows healthcare professionals to diagnose and address these issues promptly. These conditions range from infections to structural abnormalities, all of which can impact a patient’s overall health and well-being.
During the assessment, several common conditions may be identified, requiring further testing or treatment. These include:
- Infections: Such as urinary tract infections (UTIs), yeast infections, and sexually transmitted infections (STIs).
- Fibroids: Non-cancerous growths in the uterus that may cause pain or heavy bleeding.
- Cysts: Fluid-filled sacs that can develop on the ovaries, often causing discomfort or irregular periods.
- Endometriosis: A condition where tissue similar to the lining of the uterus grows outside of it, leading to pain and potential fertility issues.
- Pelvic Organ Prolapse: A condition where the pelvic organs drop lower than normal due to weakened pelvic floor muscles.
- Abnormal Pap Smear Results: Indications of potential cervical issues, including precancerous changes or HPV infection.
Identifying these conditions early can help ensure that patients receive timely care, improving outcomes and preventing the progression of more serious issues. Regular assessments are an essential part of maintaining long-term reproductive health.
Patient Communication During the Exam
Clear and effective communication with patients during a health assessment is crucial for ensuring comfort, trust, and cooperation. Open dialogue helps alleviate anxiety, clarify the procedure, and create a more positive experience for the patient. Establishing a rapport and maintaining transparency throughout the process is essential for both patient satisfaction and accurate results.
Healthcare providers should focus on the following key communication practices to enhance the experience during the procedure:
- Pre-Procedure Explanation: Clearly explain the steps of the assessment before starting. This helps the patient understand what to expect and reduces feelings of uncertainty.
- Ask for Consent: Always ask for consent before beginning any part of the procedure. Ensure that the patient feels comfortable and in control of the situation.
- Encourage Questions: Give the patient opportunities to ask questions. Address any concerns they may have to ensure they feel heard and respected.
- Check for Discomfort: Regularly check in with the patient during the procedure. Ask if they are experiencing any discomfort or pain and adjust the approach if necessary.
- Offer Reassurance: Provide calming reassurances throughout the process. Let the patient know they are doing well and that they can stop at any time if they feel uncomfortable.
- Respect Privacy: Always prioritize the patient’s privacy and dignity, ensuring that they are appropriately covered and that the room is secure.
By fostering open communication, healthcare professionals can create a supportive and respectful environment that improves the overall quality of the assessment and helps the patient feel more at ease throughout the process.
Safety Guidelines for Pelvic Examinations
Ensuring patient safety during any health assessment is paramount. Strict adherence to safety protocols minimizes risks and helps healthcare professionals perform accurate evaluations while maintaining the highest standard of care. These guidelines not only protect the patient’s physical well-being but also foster trust in the healthcare process.
Preparing the Environment
Creating a safe and comfortable environment is essential for both the patient and healthcare provider. The examination room should be clean, well-lit, and equipped with the necessary tools for the procedure. Proper sterilization of instruments is crucial to prevent infections, and a secure, private setting ensures the patient’s comfort and dignity.
Professional Conduct and Communication
Clear communication with the patient is key to ensuring safety throughout the process. Before starting, explain the procedure in detail, asking for their consent and making sure they understand each step. Always check for signs of discomfort or distress during the procedure and be prepared to stop or adjust as needed.
Key Safety Measures:
- Hygiene Practices: Wash hands thoroughly and wear gloves before conducting any physical assessment. This reduces the risk of contamination.
- Proper Positioning: Ensure the patient is positioned correctly to allow for an accurate and comfortable examination, while also ensuring their privacy is maintained.
- Monitoring the Patient’s Comfort: Regularly ask the patient if they are experiencing any pain or discomfort and adjust the procedure as necessary.
- Disinfecting Equipment: Use sterilized instruments and properly dispose of any single-use materials to prevent infections.
By following these safety guidelines, healthcare providers can minimize risks and ensure a safe, effective, and respectful examination for every patient.
Pelvic Exam Template for Routine Checkups
Regular health assessments are a vital part of maintaining long-term wellness. A well-structured approach ensures that important areas are properly evaluated, and potential health issues are detected early. These checkups serve as a preventive measure, allowing healthcare providers to monitor overall health and address any concerns that may arise.
A comprehensive routine checkup typically involves several steps designed to assess the condition of key bodily systems. The following checklist highlights the main components of such an assessment:
- Patient History: Start by reviewing the patient’s medical history, including any current symptoms, previous conditions, and family health background.
- Physical Inspection: Conduct a general physical inspection to evaluate the patient’s overall health, including posture, skin condition, and any visible signs of concern.
- Internal Assessment: Perform an internal assessment to check for any abnormalities in the reproductive system. This may include checking for cysts, fibroids, or other unusual growths.
- Laboratory Tests: Recommend any necessary lab tests such as blood work or screenings for infections or hormone levels.
- Health Advice: Based on findings, provide recommendations for maintaining health, including lifestyle adjustments, diet, or follow-up procedures if needed.
Routine checkups are essential for preventing health issues and ensuring that any emerging conditions are addressed early. A standardized approach ensures thoroughness and consistency, helping both the healthcare provider and patient stay proactive about their well-being.
Role of Pelvic Exam in Preventive Care
Routine health assessments play a critical role in early detection and prevention of potential health issues. By conducting regular screenings, healthcare professionals can identify abnormalities before they develop into serious conditions, allowing for timely interventions. These checkups are an essential part of proactive care, helping to reduce the risk of complications and improving long-term health outcomes.
Early Detection of Health Issues
One of the primary benefits of this type of assessment is its ability to detect underlying health concerns that may not yet present noticeable symptoms. Conditions such as infections, growths, or abnormalities in internal organs can be discovered early, allowing for prompt treatment and preventing further complications.
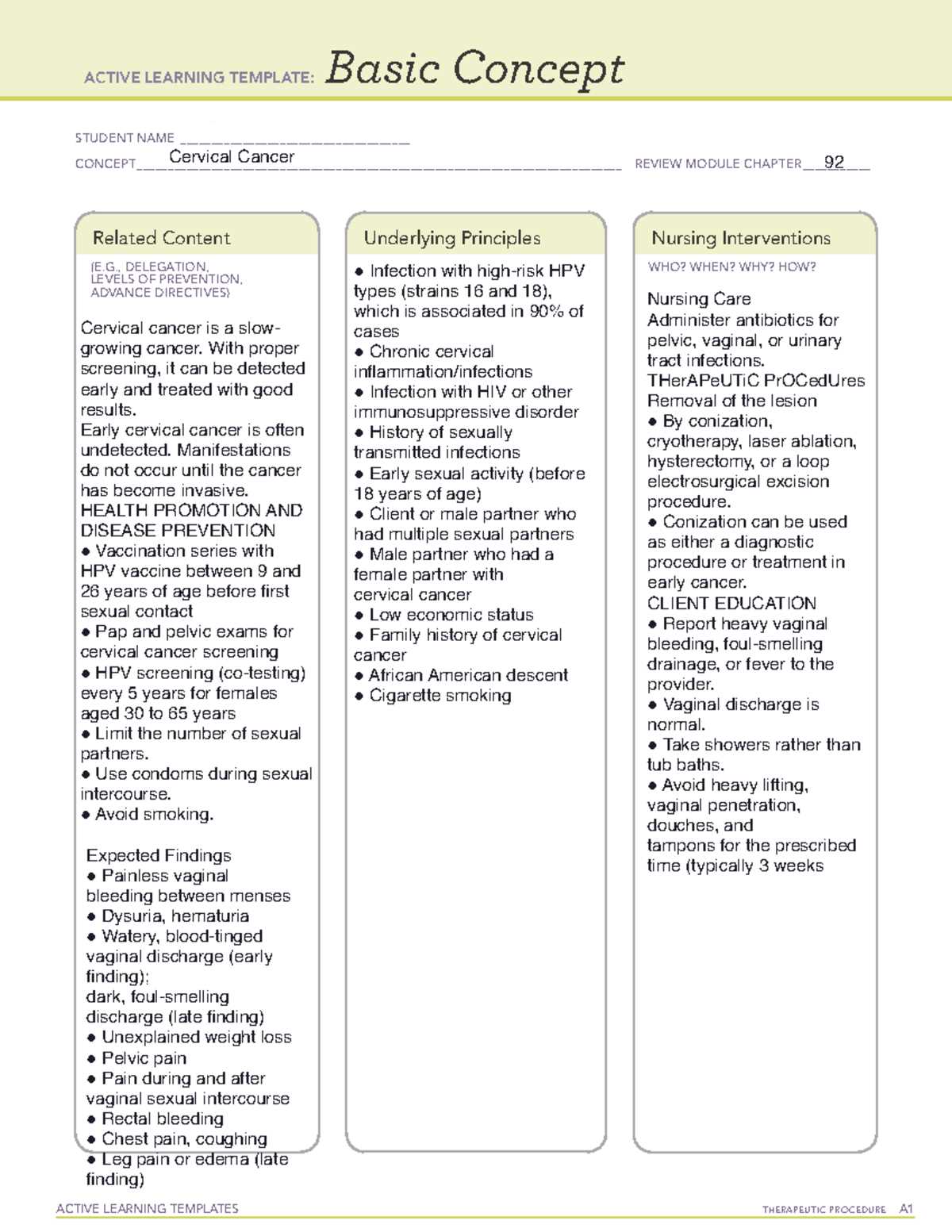
- Cervical Cancer Screening: Regular assessments help in early detection of cervical abnormalities, including precancerous cells, significantly reducing the risk of cervical cancer.
- Infections: Screening can detect infections such as sexually transmitted diseases or urinary tract infections, allowing for immediate treatment to prevent further complications.
- Reproductive Health Issues: Conditions like fibroids, cysts, or uterine abnormalities can be identified and managed before they lead to more serious complications.
Promoting Overall Wellness
In addition to detecting specific health conditions, these preventive visits also offer an opportunity to discuss overall wellness, lifestyle choices, and personal health goals. Regular consultations help maintain a strong patient-provider relationship and encourage open communication about health concerns, ensuring that patients remain engaged and proactive in their care.
- Lifestyle Recommendations: Health assessments provide the opportunity to discuss diet, exercise, and mental health, encouraging patients to adopt healthier habits.
- Emotional Support: Preventive care visits also offer emotional support, addressing any concerns or fears related to health and well-being.
By integrating these preventive screenings into regular healthcare routines, individuals can take a proactive role in safeguarding their health and well-being, benefiting from early detection and comprehensive care.
How to Address Patient Concerns
Patients often approach healthcare visits with a range of emotions, from anxiety to uncertainty. It’s essential for healthcare providers to listen actively, acknowledge their concerns, and offer clear, compassionate responses. Addressing these concerns effectively not only improves the patient experience but also helps build trust and ensure a cooperative relationship throughout the care process.
Active Listening and Empathy
Taking the time to truly understand the patient’s concerns is the first step in addressing their fears or questions. Active listening involves focusing on the patient’s words, maintaining eye contact, and refraining from interrupting. By showing empathy, you demonstrate respect for their feelings and create an environment where they feel heard and valued.
- Reassure the patient: Offer calming words to help reduce anxiety. For example, acknowledge their feelings and assure them that their concerns are valid.
- Encourage open communication: Make sure the patient feels comfortable asking questions. Provide a safe space for them to express any doubts or fears they may have.
Providing Clear Information
Patients often feel more at ease when they have a clear understanding of what to expect. By explaining procedures and answering questions in a straightforward manner, you can help alleviate uncertainty. Use simple, non-technical language and avoid jargon to ensure the patient comprehends the information fully.
- Explain the process: Walk the patient through each step of the procedure. Knowing what to expect can significantly reduce fear and make the experience more comfortable.
- Clarify any doubts: If the patient has any questions, take the time to explain the details, and offer additional resources if necessary.
By addressing patient concerns with empathy, active listening, and clear communication, healthcare providers can foster a supportive environment that empowers patients to actively participate in their own care and make informed decisions.
Training Healthcare Providers for Pelvic Exams
Proper training is essential for healthcare providers to perform sensitive procedures with competence, respect, and confidence. The quality of care during these procedures largely depends on the provider’s ability to navigate both the technical aspects and the emotional sensitivities involved. Comprehensive training ensures that healthcare professionals can conduct these assessments effectively while maintaining patient comfort and safety.
Key Aspects of Effective Training
To ensure healthcare providers are fully prepared, training should cover a range of essential skills. This includes not only technical proficiency but also communication skills, patient interaction, and ethical considerations. Providers should be educated on the latest medical guidelines, techniques, and best practices to deliver high-quality care.
- Technical Skills: Providers should be trained in the correct methods for performing assessments, ensuring accuracy and minimizing discomfort for the patient.
- Patient-Centered Communication: Training should emphasize how to explain procedures clearly, address patient concerns, and offer emotional support.
- Confidentiality and Ethical Considerations: Providers should be aware of the ethical standards that govern patient confidentiality and respect for patient autonomy during the assessment process.
Simulations and Hands-On Practice
Incorporating simulations and hands-on practice into training programs allows healthcare providers to develop their skills in a controlled environment before interacting with patients. These exercises help build confidence, reinforce the importance of patient care, and provide an opportunity to receive feedback from experienced mentors.
- Role-Playing Scenarios: Providers can practice common patient concerns and responses, preparing them for a variety of situations that may arise during real procedures.
- Hands-On Experience: Practical experience in clinical settings helps providers apply their theoretical knowledge and refine their technique under supervision.
Through ongoing education, hands-on practice, and patient-centered communication training, healthcare providers can enhance their ability to conduct these sensitive assessments safely and respectfully, ultimately improving patient outcomes and satisfaction.
Legal Aspects of Pelvic Exams
When performing sensitive medical procedures, healthcare providers must be aware of the legal implications to ensure compliance with regulations and to protect both the patient and themselves. The legal framework surrounding these procedures is designed to safeguard patients’ rights, uphold professional standards, and prevent instances of malpractice. Understanding these legal aspects is crucial for maintaining trust, ensuring ethical practices, and avoiding legal consequences.
Informed Consent
One of the fundamental legal requirements is obtaining informed consent. This ensures that the patient fully understands the procedure, its purpose, potential risks, and alternatives before agreeing to it. The healthcare provider must communicate the procedure clearly and answer any questions the patient may have, allowing them to make an informed decision about their care.
| Key Components of Informed Consent | Description |
|---|---|
| Clear Explanation | The procedure should be explained in understandable terms, avoiding medical jargon. |
| Voluntary Agreement | The patient must freely consent to the procedure without feeling coerced or pressured. |
| Right to Refuse | Patients have the right to refuse the procedure at any point without consequences. |
Confidentiality and Privacy
Confidentiality is another key legal issue. Healthcare providers are legally required to protect patient privacy and ensure that all information shared during the procedure remains confidential. Any breach of privacy could result in legal action, including malpractice claims or sanctions from medical regulatory bodies.
Additionally, patient privacy must be respected during the procedure itself, with appropriate measures in place to ensure that only those necessary for the procedure are present, and that the patient is given the opportunity to voice any concerns about their comfort and privacy.
Legal Accountability
Healthcare providers are legally accountable for their actions during the procedure. This includes ensuring that they follow the appropriate guidelines, obtain consent, and maintain a high standard of care. Failure to do so can lead to legal consequences, such as malpractice claims or disciplinary action from medical boards.
By understanding and adhering to the legal aspects surrounding these procedures, healthcare providers can minimize risk, protect patients’ rights, and maintain the integrity of the healthcare system.
Pelvic Exam for Special Patient Populations
Medical procedures must be tailored to meet the unique needs of different patient groups, especially when dealing with individuals from vulnerable or specific populations. These populations may include elderly individuals, pregnant women, adolescents, and those with disabilities, all of whom may require special consideration during medical assessments. Understanding how to adjust procedures for these groups is essential for ensuring comfort, safety, and effective care.
Considerations for Pregnant Patients
For patients who are pregnant, healthcare providers must consider both the physical changes that occur during pregnancy and the potential risks associated with certain procedures. Modifications may be necessary to ensure the well-being of both the mother and the fetus.
- Adjust positioning to avoid pressure on the abdomen.
- Limit the duration of the procedure to reduce discomfort.
- Ensure clear communication regarding the risks and benefits of any procedure.
Adapting to Elderly Patients
Older patients often have unique health concerns, including mobility issues, decreased flexibility, and chronic conditions. Healthcare providers should be mindful of these factors to make the procedure as comfortable as possible for elderly individuals.
- Use supportive devices or assistance to help with positioning.
- Be aware of frailty and adjust the intensity of the procedure accordingly.
- Provide extra time for explanations and ensure the patient feels informed and at ease.
Approaches for Adolescents
Adolescents may feel anxiety or discomfort about medical assessments, particularly if it involves sensitive procedures. It’s crucial to create a comfortable environment and offer reassurance.
- Use age-appropriate language and explanations.
- Involve a guardian or trusted person for support during the procedure.
- Provide privacy and ensure that the adolescent feels in control of the situation.
Patients with Disabilities
Patients with disabilities may face physical or cognitive challenges that require accommodations during medical procedures. Providers should be patient and flexible in their approach to ensure that these patients receive appropriate care.
- Modify positions or use adaptive equipment for those with mobility challenges.
- Ensure clear communication and offer assistance if needed for those with cognitive impairments.
- Take extra time to ensure the patient understands the procedure and is comfortable.
Adapting procedures for special patient populations is essential for delivering personalized and compassionate care. By considering the unique needs of these groups, healthcare providers can foster trust, minimize discomfort, and improve overall outcomes.
Utilizing Technology in Medical Assessments
The integration of modern technology in healthcare has significantly transformed the way medical professionals conduct assessments and monitor patient health. From diagnostic imaging tools to advanced monitoring systems, technology provides essential support in improving accuracy, efficiency, and patient comfort. In sensitive procedures, the use of technological innovations can also enhance communication, provide more precise results, and allow for less invasive methods, all contributing to a better overall healthcare experience.
Digital Imaging and Diagnostic Tools
One of the key advancements in medical assessments is the use of digital imaging. Tools such as ultrasound and other imaging devices allow for detailed, real-time visualization of internal structures. These technologies not only help in diagnosing conditions but also in guiding healthcare professionals during procedures, ensuring higher precision and reducing the need for invasive techniques.
- Provides clear, immediate images that help identify abnormalities.
- Enables non-invasive monitoring of internal structures over time.
- Allows healthcare providers to make more informed decisions based on visual data.
Electronic Health Records (EHR) and Data Management
The use of Electronic Health Records (EHR) has streamlined the documentation and sharing of patient information. With real-time access to medical histories, test results, and treatment plans, providers can offer more personalized care. EHRs also improve the accuracy of record-keeping and help reduce the risk of errors during procedures, ensuring that all necessary data is accessible when needed.
- Enables healthcare providers to access patient data quickly and securely.
- Improves accuracy and reduces paperwork during assessments.
- Facilitates better communication between specialists and care teams.
As technology continues to evolve, its role in enhancing patient care and improving medical procedures will expand further. By leveraging these advancements, healthcare professionals can provide more effective, efficient, and patient-centered services.
Improving Patient Comfort During the Procedure
Ensuring that patients feel comfortable and at ease during medical procedures is essential to providing effective care. Anxiety and discomfort can interfere with the quality of the examination, potentially leading to inaccurate results or patient reluctance to follow up with necessary care. By implementing thoughtful strategies and enhancing communication, healthcare providers can significantly improve the patient’s experience and overall satisfaction.
Creating a Relaxing Environment
One of the first steps in improving comfort is the physical environment. A quiet, well-lit, and private space helps to reduce patient anxiety. Soft lighting, calm music, and a clean, organized room can create a more inviting atmosphere. In addition, providing comfortable seating and maintaining a temperature that suits the patient helps them feel more relaxed before and during the procedure.
- Maintain privacy and confidentiality at all times.
- Ensure the room temperature is comfortable for the patient.
- Offer calming music or background sounds to reduce stress.
Effective Communication and Support
Clear and compassionate communication plays a crucial role in easing patient nerves. Healthcare providers should explain the procedure in detail, including what the patient can expect at each stage. Allowing patients to ask questions and express any concerns before the procedure helps them feel more in control. Additionally, offering reassurance during the process can alleviate discomfort and build trust.
- Explain each step before proceeding to ensure the patient understands.
- Encourage questions and actively listen to any concerns.
- Provide gentle reassurances during the procedure to maintain comfort.
By integrating these strategies, healthcare professionals can improve both the patient experience and the overall effectiveness of the procedure, fostering a more trusting and positive relationship between provider and patient.
Reviewing and Updating Clinical Protocols
Regularly reviewing and updating clinical documentation is essential to ensure that medical procedures are carried out efficiently and effectively. With new research, medical advancements, and evolving patient needs, it is important for healthcare providers to maintain up-to-date guidelines that align with the latest standards of care. This process involves evaluating current protocols, making necessary adjustments, and implementing changes that enhance both the accuracy of the procedure and patient comfort.
Evaluating Existing Protocols
The first step in updating clinical protocols is a thorough evaluation of the current guidelines. This involves reviewing existing practices to identify areas that may need improvement. Feedback from healthcare providers, patient outcomes, and recent advancements in medical research should be considered to ensure the protocols are still relevant and effective. Regular audits and discussions among the healthcare team can highlight any gaps or inefficiencies that need addressing.
- Gather feedback from clinical staff and patients.
- Review patient outcomes and satisfaction surveys.
- Monitor recent medical literature for best practices and innovations.
Implementing Necessary Changes
Once areas for improvement have been identified, it is essential to implement changes to the protocols. This may include updating language for clarity, adding new steps or procedures, or revising existing techniques based on the latest evidence. Training healthcare providers on these updates ensures that the new procedures are effectively integrated into daily practice. Additionally, it is important to regularly revisit these protocols to ensure they remain aligned with evolving healthcare standards and patient needs.
- Revise and update procedural steps as necessary.
- Ensure all staff are trained on updated protocols.
- Schedule regular reviews to keep guidelines current.
By continuously reviewing and refining clinical protocols, healthcare providers can enhance the quality of care, reduce errors, and improve overall patient experiences. An ongoing commitment to improvement ensures that both patients and healthcare professionals benefit from the best practices available.