Comprehensive Mental Status Exam Training for Professionals
In clinical practice, evaluating a patient’s psychological state is a crucial part of the diagnostic process. Professionals must be able to assess various cognitive and emotional aspects to understand the overall well-being of an individual. These evaluations help in identifying potential disorders and determining appropriate treatment plans. The ability to conduct thorough assessments requires not only knowledge but also practical experience to accurately interpret signs and symptoms.
Developing proficiency in psychological assessments involves mastering techniques that involve careful observation and detailed questioning. Through focused training, clinicians can learn how to evaluate different dimensions of a person’s mental health, such as thought patterns, mood stability, and perception. These skills contribute to making more informed decisions, improving patient outcomes, and building trust in therapeutic relationships.
Understanding the Mental Status Evaluation
Conducting a thorough assessment of a person’s psychological condition is fundamental in identifying and understanding their cognitive and emotional state. This process provides insights into an individual’s thinking, mood, perception, and behavior, helping professionals make accurate clinical judgments. By observing and questioning, clinicians can gather essential information to form a comprehensive understanding of the patient’s mental health.
Key aspects of this evaluation involve assessing various domains such as awareness, speech patterns, and emotional responses. Understanding how these elements interact is crucial for diagnosing conditions like depression, anxiety, and cognitive disorders. Effective evaluation requires both structured methods and intuitive insights based on experience.
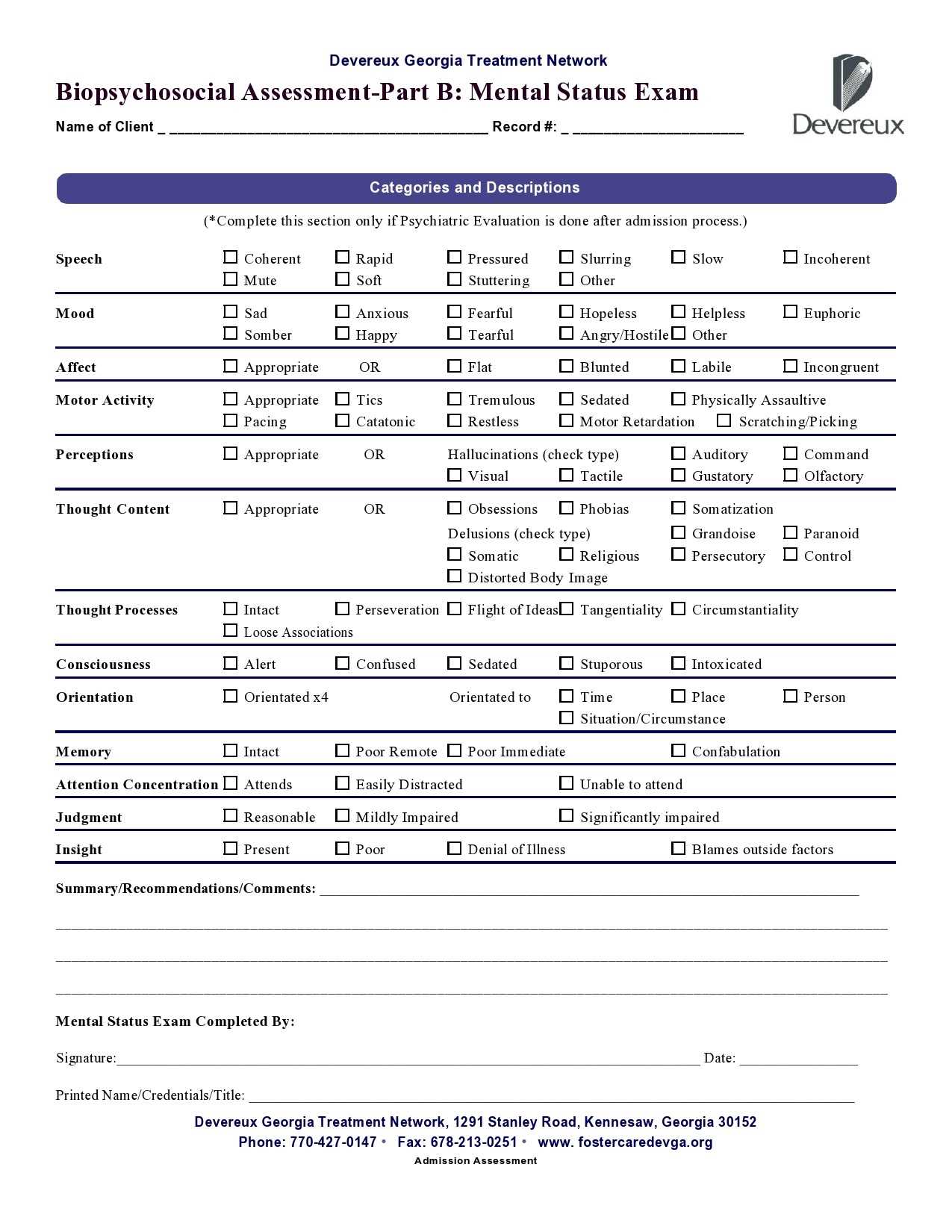
| Area of Evaluation | Description |
|---|---|
| Appearance and Behavior | Observing physical state, hygiene, posture, and movement patterns. |
| Cognitive Functioning | Assessing memory, attention span, and problem-solving abilities. |
| Emotional State | Evaluating mood, affect, and emotional reactions. |
| Speech and Language | Examining fluency, coherence, and appropriateness of speech. |
| Perception and Thought Content | Understanding any delusions, hallucinations, or unusual thoughts. |
Key Components of the Psychological Assessment
A comprehensive psychological evaluation involves examining several critical aspects of a person’s cognitive and emotional state. These components help clinicians gather necessary data to understand how the individual is functioning mentally and emotionally. By focusing on each area, professionals can assess a wide range of conditions and gain insights into the patient’s overall well-being.
Each element plays a unique role in the process. The first step is often to assess the patient’s appearance and behavior, which includes physical traits and observable actions. Next, cognitive abilities such as memory, attention, and problem-solving are carefully evaluated to understand mental processes. Emotional responses, speech patterns, and thought content also provide crucial clues to the patient’s mental health status. By examining these factors in depth, clinicians can build a more accurate picture of the individual’s psychological state.
Why the Psychological Evaluation Matters
Conducting a thorough psychological assessment is essential for understanding a patient’s mental and emotional well-being. It allows healthcare professionals to identify underlying conditions, track changes over time, and make informed decisions about care plans. Without this key step, accurate diagnosis and effective treatment can become challenging.
By performing a detailed evaluation, clinicians can uncover a range of important factors, including:
- Identifying cognitive impairments or disorders
- Recognizing emotional instability or mood disturbances
- Understanding how a patient perceives reality and interacts with their environment
- Assessing the impact of mental health on daily functioning
- Helping to tailor therapeutic interventions to the individual’s needs
A well-conducted evaluation also serves as a baseline for future assessments, helping to measure progress and adjust treatments as necessary. For professionals in the field, these assessments are an indispensable tool in delivering effective, patient-centered care.
Common Errors in Psychological Assessment
When conducting a psychological assessment, it’s easy to make mistakes that can lead to inaccurate conclusions. These errors can affect the quality of care provided to patients and complicate diagnosis. It’s important for professionals to recognize these common pitfalls and take steps to avoid them in order to ensure reliable results.
Overlooking Subtle Symptoms
One common mistake is failing to identify subtle signs of mental health issues. Symptoms like mild anxiety or early cognitive decline may not be immediately apparent, but they can have a significant impact on a patient’s overall well-being. It’s crucial to look beyond obvious behaviors and pay attention to more nuanced changes in mood, speech, or thought processes.
Bias and Assumptions in Assessment
Another frequent error is allowing personal biases or assumptions to influence the assessment process. Clinicians may unintentionally interpret behaviors or responses based on stereotypes or past experiences. To avoid this, it’s essential to remain objective and approach each patient as an individual, without making judgments based on preconceived notions.
Building Confidence with Psychological Assessments
Gaining confidence in conducting psychological evaluations is essential for providing accurate and reliable insights into a patient’s condition. As with any clinical skill, consistent practice and a structured approach can greatly enhance a clinician’s ability to perform these assessments effectively. Confidence comes not only from experience but also from understanding the key components and staying mindful of potential challenges.
Here are a few strategies to build confidence when conducting assessments:
- Familiarize yourself with the common signs and symptoms of various mental health conditions.
- Practice active listening and observation techniques to detect subtle changes in behavior.
- Start with structured assessments and gradually adapt to more fluid, conversational approaches as you gain comfort.
- Seek feedback from colleagues or supervisors to refine your skills.
- Review past cases and reflect on areas of improvement to identify patterns and develop insights.
Building confidence takes time, but by following these strategies, clinicians can improve their evaluation techniques and become more skilled in assessing a wide range of conditions.
Essential Skills for Conducting Assessments
Successfully performing psychological evaluations requires a variety of skills that go beyond simply asking questions. Clinicians must be able to observe, analyze, and interpret various aspects of a patient’s behavior and cognitive functioning. These abilities are crucial for gaining accurate insights and making informed decisions about treatment and care.
Observational Skills
The ability to observe and accurately interpret a patient’s behavior is fundamental in any psychological assessment. Clinicians should be able to detect subtle changes in mood, motor activity, and facial expressions, which can provide valuable clues about underlying mental health issues. This skill requires patience and attention to detail, as non-verbal cues often speak volumes about a person’s emotional state.
Effective Communication
Clear and effective communication is another essential skill. Clinicians need to establish trust with their patients and encourage open dialogue. Asking the right questions in a calm and empathetic manner helps to gather relevant information while ensuring the patient feels comfortable. Additionally, being able to communicate findings with other healthcare providers is crucial for coordinating care and treatment plans.
How to Observe Patient Behavior Effectively
Observing a patient’s behavior is an essential part of understanding their emotional and cognitive state. Effective observation involves more than simply watching for overt actions; it requires careful attention to subtle cues, context, and patterns of behavior that may indicate deeper psychological or physiological issues. Skilled clinicians can gather valuable insights from body language, speech, and interactions, which can significantly aid in diagnosis and treatment planning.
To observe behavior effectively, it’s important to focus on both verbal and non-verbal signals. Body posture, facial expressions, eye contact, and tone of voice all provide important information about a patient’s emotional and mental state. At the same time, listening carefully to the patient’s words, as well as how they speak, can reveal cognitive functioning and mood stability. Context is also key–understanding the environment and circumstances surrounding the behavior ensures that observations are interpreted accurately.
| Behavioral Aspect | What to Look For |
|---|---|
| Posture and Movement | Rigid, slouched, or restless movements can indicate emotional tension, anxiety, or depression. |
| Facial Expressions | Unexpressive or exaggerated facial gestures may signal emotional detachment or heightened stress. |
| Speech Patterns | Speed, clarity, and tone of speech can reflect cognitive clarity, mood, and emotional state. |
| Eye Contact | Frequent avoidance may suggest discomfort or anxiety, while excessive eye contact could indicate aggression or overstimulation. |
Interpreting Cognitive Function in Assessments
Assessing cognitive function is a critical part of understanding a patient’s mental processing capabilities. By evaluating areas such as memory, attention, and reasoning, clinicians can gain valuable insights into the patient’s cognitive health. Cognitive assessments help identify potential issues such as cognitive decline, neurological conditions, or the impact of mental health disorders on a person’s ability to think and process information effectively.
Memory and Recall
Memory plays a central role in cognitive function, and any disturbances can be an important indicator of underlying issues. When assessing memory, it is crucial to distinguish between short-term and long-term recall. Difficulty remembering recent events or forming new memories may suggest cognitive impairment, while problems with long-term memory could point to more severe conditions such as dementia. Asking patients to recall details or perform tasks that require both recent and remote memory is essential for a comprehensive evaluation.
Attention and Concentration
Another key aspect of cognitive function is a patient’s ability to focus and maintain attention. Difficulty sustaining attention may indicate cognitive disorders such as ADHD, or it could be a sign of emotional distress, such as anxiety or depression. During the assessment, clinicians may ask patients to perform simple tasks that require focus, such as repeating back sequences of numbers or performing tasks with multiple steps. The ability to stay on task and avoid distractions is a critical indicator of cognitive health.
Assessing Mood and Affect During Evaluations
Evaluating a patient’s mood and emotional expression is a fundamental part of understanding their psychological state. Mood refers to the overall emotional tone a person experiences, while affect describes the outward expression of those emotions. By observing these aspects, clinicians can gain insights into the emotional well-being of a patient and identify any signs of disturbances such as depression, anxiety, or mood disorders.
Recognizing Emotional Tone
During the evaluation, it’s important to gauge the patient’s emotional tone. A patient’s mood can range from elevated and euphoric to flat or depressed. Changes in mood, especially those that are extreme or out of proportion to the situation, can be indicators of underlying conditions such as depression, bipolar disorder, or other mood disturbances. Clinicians should pay attention to both verbal and non-verbal cues, such as the patient’s choice of words, tone of voice, and general demeanor.
Observing Emotional Expression
Affect is assessed by observing how emotions are expressed externally. It is important to look for congruence between a person’s stated mood and their facial expressions, gestures, and body language. For example, a person describing feelings of happiness but showing signs of sadness through their expression may be experiencing an emotional disconnect or may be masking their true feelings. A clinician should consider whether the affect is appropriate, blunted, or restricted, as these could indicate significant psychological conditions.
Evaluating Thought Processes in Patients
Assessing a patient’s thought processes is essential for understanding their cognitive functioning and emotional well-being. The way a person thinks can reveal important information about their ability to reason, organize ideas, and form coherent conclusions. Disorganized or illogical thinking can be a sign of underlying psychological or neurological issues, which is why careful evaluation is necessary to identify potential disorders such as schizophrenia, anxiety, or other cognitive impairments.
When evaluating thought processes, clinicians must look for signs of coherence, clarity, and logical flow in the patient’s speech and ideas. Disruptions in thinking can manifest as tangential speech, incoherent thought patterns, or illogical conclusions. In addition to listening to the content of what a patient says, it’s important to consider how they say it, as speech patterns can provide valuable insight into the quality of their thinking.
Key Areas to Observe in Thought Process Evaluation:
- Coherence and Organization: The ability to connect thoughts logically and stay on topic is a critical indicator of cognitive health.
- Clarity of Expression: Patients should be able to express their thoughts clearly. Difficulty with articulation or word-finding may signal cognitive issues.
- Presence of Disorganized Thinking: Watch for signs of fragmented or disconnected thoughts, which may indicate a disorder like schizophrenia.
Role of Insight and Judgment in Evaluations
In clinical assessments, understanding a patient’s insight and judgment is crucial for evaluating their overall cognitive functioning and awareness. Insight refers to a person’s ability to recognize and understand their own condition, while judgment involves the capacity to make sound decisions based on reasoning and circumstances. Both of these factors are integral in identifying how well a patient grasps their own mental health, as well as their ability to navigate daily life and make appropriate choices.
Assessing insight and judgment provides valuable clues about the severity of a condition and its impact on the patient’s ability to function effectively. For instance, a person with poor insight may be unaware of their illness or deny the need for treatment, while impaired judgment could lead to risky behaviors or poor decision-making. Clinicians should evaluate these aspects carefully to determine how much a patient can understand and manage their circumstances.
- Insight: Evaluate whether the patient understands their condition and is aware of the effects it may have on their life.
- Judgment: Observe how the patient makes decisions and assess whether those decisions are rational and appropriate for their situation.
- Practical Examples: Asking the patient hypothetical situations can reveal their decision-making process and level of insight into their actions.
Understanding Perceptions and Delusions
In clinical assessments, understanding a patient’s perceptions and beliefs is essential for identifying possible cognitive or psychological disturbances. Distorted perceptions and false beliefs can significantly impact a person’s behavior, relationships, and overall functioning. By evaluating how patients interpret the world around them, clinicians can gain insight into underlying conditions such as psychosis, schizophrenia, or other thought disorders.
Recognizing Distorted Perceptions
Distorted perceptions can manifest in various forms, such as hallucinations, where the patient may perceive things that are not present, or misinterpretation of sensory input. For example, a patient may hear voices that others do not hear or see things that do not exist. These perceptual disturbances can significantly affect the individual’s reality, and recognizing them early is crucial for effective treatment.
Identifying Delusions
Delusions are false beliefs that are strongly held, despite evidence to the contrary. These beliefs can be paranoid, grandiose, or bizarre, and often lead to behaviors that are out of touch with reality. For example, a person may believe they are being persecuted or have special powers. Identifying delusions is important because it helps determine the severity of a patient’s condition and guides treatment planning.
Ethical Considerations in Mental Health Assessments
When conducting evaluations in mental health settings, ethical issues play a critical role in ensuring the process is respectful, fair, and protective of patients’ rights. It is essential for clinicians to approach these assessments with a clear understanding of their professional responsibilities, ensuring that patient autonomy, confidentiality, and informed consent are upheld throughout the evaluation. Ethical dilemmas can arise when balancing the need for accurate information with the need to respect a patient’s dignity and privacy.
Informed Consent and Patient Autonomy
One of the primary ethical concerns in any assessment is obtaining informed consent. This involves explaining the purpose, nature, and potential consequences of the evaluation to the patient in a manner they can understand. Patients must have the autonomy to decide whether to participate, and their consent should be voluntary. This is particularly important when dealing with vulnerable populations, such as individuals with cognitive impairments or mental health disorders that may affect their decision-making abilities.
Maintaining Confidentiality and Privacy
Confidentiality is another key ethical principle that must be adhered to during any clinical assessment. The information gathered from a patient should be treated with the utmost confidentiality, ensuring it is shared only with those who have a legitimate need to know. Ethical concerns can arise if information is disclosed without proper consent or if it is used for purposes other than the intended clinical evaluation.
| Ethical Principle | Description |
|---|---|
| Informed Consent | Ensuring the patient understands the evaluation process and consents voluntarily. |
| Autonomy | Respecting the patient’s right to make their own decisions regarding participation. |
| Confidentiality | Protecting the patient’s private information from unauthorized disclosure. |
Training Techniques for Mental Health Professionals
Effective preparation for healthcare providers in mental health settings is essential for delivering high-quality care and ensuring proper patient evaluations. Specialized training techniques help professionals develop the skills needed to accurately assess and understand patient behaviors, emotions, and thought processes. These approaches enhance clinical competency and ensure that practitioners can identify, assess, and address complex psychological conditions with confidence and empathy.
Simulation-Based Learning
One of the most effective methods for building proficiency in clinical evaluations is through simulation-based learning. This technique allows professionals to practice their skills in a controlled, realistic environment, with the opportunity to respond to a variety of patient scenarios. By engaging in role-playing exercises, healthcare providers can better understand patient reactions and refine their techniques for handling different psychological conditions.
Supervised Practice and Feedback
Another critical technique for improving evaluation skills is supervised practice, where trainees conduct assessments under the supervision of experienced mentors. This approach provides real-time feedback and guidance, allowing professionals to learn from their mistakes and refine their methods. The mentor’s role is to offer constructive feedback, highlight areas for improvement, and reinforce best practices to ensure that professionals are prepared for independent clinical work.
Using Case Studies to Improve Skills
Incorporating case studies into professional development is a powerful method for enhancing clinical skills. By analyzing real-world scenarios, healthcare professionals can apply theoretical knowledge to practice, sharpening their decision-making and assessment abilities. Case studies allow trainees to explore complex situations and challenges that may arise during patient evaluations, helping them better understand the nuances of various psychological conditions and responses.
Analyzing Real-World Scenarios
Case studies provide a detailed look at actual patient encounters, offering professionals the chance to observe how different factors influence the outcome of an assessment. By reviewing specific patient histories, behaviors, and symptoms, clinicians can better grasp the importance of context in understanding a patient’s condition. This analytical approach promotes critical thinking and helps professionals improve their ability to make informed decisions when faced with similar situations in the future.
Learning from Expert Feedback
Another benefit of using case studies is the opportunity to receive feedback from experienced mentors. In many training environments, case studies are discussed in group settings where trainers and peers can provide insights and suggestions. This collaborative learning process allows professionals to consider alternative perspectives, enhancing their problem-solving abilities and reinforcing best practices in patient evaluation.
Tools and Resources for Effective Assessment
To conduct thorough and accurate evaluations, healthcare professionals rely on various tools and resources that facilitate the assessment process. These instruments are designed to provide structure, enhance reliability, and ensure that critical aspects of patient health are not overlooked. By using a combination of standardized tests, digital platforms, and reference materials, professionals can enhance their skills and ensure more accurate diagnoses.
Standardized Assessment Tools
Standardized instruments are essential for ensuring consistency and objectivity in evaluations. These tools provide structured frameworks for assessing different aspects of a patient’s condition, helping professionals gather reliable data in a systematic way. Some commonly used tools include:
- Cognitive Assessment Tools: Instruments that assess memory, attention, and other cognitive functions.
- Self-Report Questionnaires: Tools that allow patients to express their own perceptions of their mental health.
- Behavioral Rating Scales: Scales designed to assess specific behaviors, such as anxiety, depression, or mood swings.
Digital Platforms and Software
In today’s healthcare landscape, digital platforms and software have become integral to the assessment process. These tools enable professionals to collect, analyze, and store patient data more efficiently. Features such as automatic scoring, trend analysis, and secure data storage enhance the accuracy and accessibility of assessments. Examples include:
- Electronic Health Records (EHR): Systems that store patient data and assessment results, facilitating communication and follow-up.
- Assessment Management Software: Platforms that help track and manage the progression of patient evaluations over time.
Reference Materials and Guidelines
Comprehensive reference materials, such as textbooks, clinical guidelines, and research papers, play a critical role in shaping effective assessment practices. By staying informed about the latest research and guidelines, professionals can ensure that their methods align with current best practices and evidence-based standards. Key resources include:
- Clinical Handbooks: Guides that provide a framework for conducting specific assessments.
- Research Journals: Peer-reviewed articles that offer insights into emerging techniques and best practices in the field.
Improving Diagnostic Accuracy through Practice
Diagnostic accuracy plays a crucial role in providing effective patient care. One of the most effective ways to enhance this accuracy is through regular practice and experience. As healthcare professionals refine their observation skills and become more familiar with the nuances of patient assessments, their ability to make precise and reliable evaluations improves. This section focuses on how ongoing practice can lead to better diagnostic outcomes.
Building Confidence Through Repetition
Repetition helps solidify the core principles of patient assessment, allowing professionals to become more confident and efficient in their decision-making. Regular practice helps to sharpen attention to detail and ensures that important symptoms are not overlooked. Methods for improving diagnostic accuracy through repetition include:
- Regular Case Studies: Reviewing a variety of patient scenarios to familiarize oneself with diverse conditions and symptoms.
- Simulation Exercises: Participating in mock assessments that mimic real-world patient interactions, helping to build familiarity and confidence.
- Peer Review and Feedback: Engaging with colleagues to review assessments and receive constructive feedback, allowing for continuous improvement.
Refining Skills with Ongoing Learning
Diagnostic skills are continuously evolving, and staying updated with new research, methodologies, and techniques is vital. Professionals who engage in ongoing learning are better equipped to interpret patient data accurately. Strategies for improving diagnostic accuracy through learning include:
- Continuous Education: Attending workshops, webinars, or courses to stay informed about the latest advancements in diagnostic practices.
- Reading Medical Journals: Regularly reviewing peer-reviewed articles to gain insights into the latest research and clinical guidelines.
- Mentorship and Supervision: Working alongside experienced practitioners who can provide guidance and share best practices for accurate assessments.